INTRODUCTION
Rifampicin is a first-line anti-tuberculosis antibiotic drug used to treat Mycobacterium tuberculosis. It inhibits the P subunit of bacterial RNA polymerase with a consequent inhibition of messenger RNA 1 ; its use can generate side effects, including liver and gastrointestinal involvement and acute kidney injury, which was reported in 0.05% of patients in a retrospective study conducted between 1987 and 1995. 2 Factors associated with increased risk of kidney involvement were reintroduction and intermittent use of rifampicin. 2,3
The onset of acute kidney injury in patients using rifampicin for the first time has been barely reported in the literature. 4 These people have a favorable prognosis for recovery of kidney function, which can range from 73% 5 to 96% 2, while mortality can reach up to 1.6%. 2
CASE PRESENTATION
A 32-year-old Hispanic male from Venezuela and living in Bogotá D.C., unemployed and with scarce socioeconomic resources, was admitted to the emergency department of the Hospital Universitario Mayor Méderi after being referred for outpatient treatment of tuberculosis. Treatment was started one month prior to consultation according to the four-drug fixed-dose combination regimen used to treat this condition (isoniazid, rifampin, pyrazinamide, and either ethambutol or streptomycin). 6
The patient's kidney function was normal prior to antituberculosis management and he had no previous exposure to other medications, but given the abnormal results of laboratory tests regarding kidney function, he was referred to the emergency department. On admission, the patient was in good general condition; hydrated; without rashes, fever, dysuria, hematuria, abdominal pain, nausea, vomiting, fatigue, or decreased or increased amount of urine; he did not present any other symptoms on review of systems, nor manifested other relevant medical history. Physical examination revealed heart rate of 78 beats per minute, respiratory rate of 18 breaths per minute, and blood pressure of 118/68 mmHg. Fist percussion was negative and there was no abdominal pain, edema, or neurological abnormalities.
Creatinine test requested by the outpatient consultation service had values of 4.17 mg/dL. On admission, new tests were performed (Table 1), which showed elevated azoids, proteinuria in non-nephrotic range and metabolic acidosis with increased anion gap; lactic acidosis and diabetic ketoacidosis were ruled out as causes of these symptoms.
Table 1 Laboratory test results on admission.
| Test | Results |
|---|---|
| Blood count | Leucocytes: 5 460, neutrophils: 3 750, lymphocytes: 840, eosinophils: 100, hemoglobin: 10.1 mg/dl, hematocrit: 31%, mean corpuscular volume: 83.3fL, mean corpuscular hemoglobin: 32pg, red blood cell distribution width: 16.8%, platelets: 360 000. |
| Urinalysis | Specific gravity: 1 008, pH: 5, proteins: 25 mg/dL, glucose: 100 mg/dL, red blood cells: 25xc, leucocytes: 5 xc, scarce bacteria and no eosinophiluria. |
| Electrolytes | Sodium: 136 mmol/L, potassium: 4.6 mmol/L, chlorine: 103 mmol/L, magnesium: 2.05 mmol/L. |
| Others | Prothrombin time: 16.1 s, thromboplastin time: 23 s, human immunodeficiency virus: negative, hepatitis b surface antigen: negative, hepatitis c antibodies: negative, cultures: negative. |
| Test | Results |
| Arterial blood gases | pH: 7.38, partial pressure of oxygen: 86, partial pressure of carbon dioxide: 23, bicarbonate: 14, base excess: -9.4, lactate 1, ratio of partial pressure arterial oxygen and fraction of inspired oxygen: 41 5. |
| Additional | 24-hour urine protein: 700 mg/dL, urine sodium: 99 meq/L, urine potassium: 19.6 meq/L, urine chlorine: 78.1 meq/L, glucose: 102mg/dL. |
| Immunological | Antinuclear antibodies: negative, anti-DNA: negative, anti-LA: negative, anti-RO: negative, anti-SM: negative, anti-RNP: negative, C3: normal, C4: normal, anti-neutrophil cytoplasmic antibodies: negative. |
Source: Own elaboration.
Kidney and urinary tract ultrasound showed normal-sized kidneys with diffuse increase in echogenicity and no loss in corticomedullary differentiation.
The patient presented acute kidney disease KDIGO III 7, glomerular filtration rate of 23.38 mL/min calculated by cockroft, proteinuria in the non-nephrotic range, high anion gap metabolic acidosis, urine sediment with glycosuria, positive urine anion gap and normal central glucose. All this led to consider that there was proximal tubular involvement compatible with Fanconi syndrome.
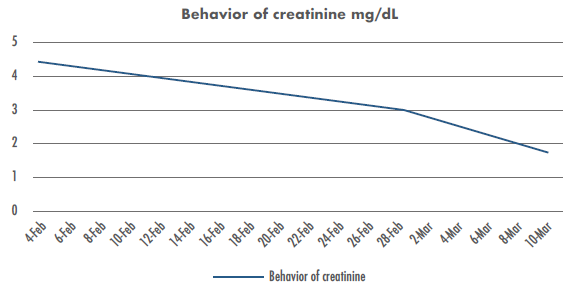
Considering the acute renal injury with proximal and distal tubular involvement, the history of tuberculosis and that rifampicin is the most frequently involved drug in kidney failure in this type of cases 8, treatment was suspended and a kidney biopsy was indicated to confirm the origin of the failure and plan a treatment. After the suspension of rifampicin, azotemias improved until creatinine was normalized (Figure 1).
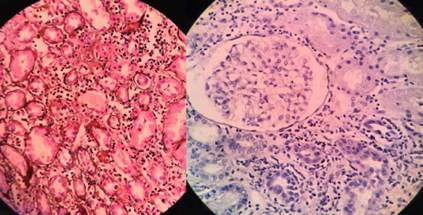
Kidney biopsy confirmed acute tubuloint- erstitial nephritis (ATIN) with inflammatory cells, eosinophils, and interstitial edema. The findings were also suggestive of drug hypersensitivity with associated tubular injury (Figure 2).
Figure 2 shows 23 normal glomeruli with normal basement membrane, no mesangial expansion and no endocapillary or extracapillary proliferation. Tubulointerstitial findings included: interstitial inflammation of the whole cortical area; presence of mononuclear inflammatory cells (+ + + +); eosinophils (++); plasmocytes (++); tubulitis (++) with focal rupture; degenerative changes of the tubular epithelium; detachment, flattening and cellular remains at intraluminal level with some neutrophils; extensive irregular vacuolization of the tubular epithelium; and irrelevant vascular findings that did not show sclerosis or hyalinosis.
Management with prednisolone at 1 mg/kg was initiated with stabilization of kidney function after 6 weeks. Once creatinine levels normalized (0.9 mg/dl), the patient was discharged; he continued with antituberculosis treatment and tests for follow-up of kidney function.
DISCUSSION
ATIN is defined as an infiltration of inflammatory cells into the renal interstitium that leads to oliguric or non-oliguric kidney injury and causes up to 27% of sudden kidney failures. 9 The causes may be allergic, infectious, autoimmune, systemic, idiopathic or drug-induced. 5,10
Drug-induced ATIN is the most common form found in practice (up to 1/3 caused by antibiotics) and is characterized by a classic clinical triad (rash, fever, and urine eosinophils), occurring in less than 10% of patients. When it only shows kidney manifestations, this infiltration has a worse prognosis and its diagnosis is late, so in most cases it requires treatment with steroids. 11 Therefore, when it is suspected, a kidney biopsy, which is the gold standard for diagnosis, is necessary. 8,12
Rifampicin rarely causes ATIN and its onset is associated with irregular drug intake or systemic symptoms of hypersensitivity. 9 On its physiopathological mechanism, antigen I, which is found in red blood cells and tubular cells, generates a response associated with immunoglobulin M and, to a lesser extent, with agglutination by immunoglobulin G in the presence of rifampicin. When the same response is obtained in vitro without the drug, such agglutination is not observed. 12
Fanconi syndrome is an inherited or acquired disorder in the proximal renal tubules that results in excretion of amino acids, phosphate, bicarbonate and glucose. 13,14 Urine anion gap is a useful tool to diagnose distal tubular involvement and to differentiate some of its causes, such as diarrhea, in patients with metabolic acidosis. It is calculated using the formula urine sodium + urine potassium - urine chlorine, and is considered positive when the value is between 20 and 90 15; in the reported patient, the value of this anion was 40.
Although the patient was asymptomatic, ATIN diagnosis was achieved based on the findings in urine sediment, the temporal relationship with the administration of anti-tuberculous drugs, and the fact that rifampicin is the drug most associated with this pathology. 8,16
Some publications on this subject can be found in the literature. Chang et al.5, in a study conducted in Taiwan, studied acute kidney disease in patients treated with the four-drug tuberculosis regimen and found that it occurred in 7.1% of patients, of whom 11% developed the disease after first exposure to rifampicin. Muthukumar et al.3 published a case series of 25 patients with acute kidney disease secondary to the use of rifampicin; the patients presented with oliguria, and the most common histological finding was ATIN, which might be associated with anemia (96%), hemolysis (1 7%) and thrombocytopenia (50%), and could help create a diagnostic approach and reach clinical suspicion. 2 Given that Bogotá is located more than 2 600 meters above sea level, and that the reported patient was anemic, the associated physiopathology correlated with antigen I. 12 Finally, the study by Schubert et al.8, conducted between 1995 and 2007, evaluated the clinical features and complications of ATIN treated with the four-drug TB regimen, which was typically associated with re-exposure to the drugs; AITN occurred in 5% of patients and had a presentation range of 1 to 21 days after the initiation of the treatment. 8
The literature reviewed in PubMed and SciELO did not report any other cases of ATIN by rifampicin in Colombia, but there were contradictory results with respect to treatment for this disease with steroids. The review by González et al.17 suggests significant improvement in kidney function, while Effa et al.18 did not find any difference regarding the improvement of kidney function. No case reported the use of a defined dose of steroids, and the studies on which systematic reviews were conducted were very heterogeneous, mostly retrospective case reviews. In this patient, it was decided to start treatment with steroids for 6 weeks at 1 mg/kg, after which outpatient treatment was continued with complete recovery of kidney function.
CONCLUSIONS
Since there are few reported cases of ATIN in Latin America and it is a rare complication associated with rifampicin use, this case report is useful as it warns clinicians to suspect this disorder in patients who initiate or restart anti-tuberculous treatment and have subsequent kidney failure. To confirm the suspicion, further studies evaluating the effectiveness of steroids in ATIN by rifampicin at defined doses in high-prevalence tuberculosis settings should be conducted in order to define the usefulness of steroid use.