INTRODUCTION
Falls are a common problem among patients over 60 years of age and are caused by multiple reasons; therefore, it has been necessary to implement specific protocols aimed at managing this problem, which include scales for predicting falls, and study and management protocols. 1 Novel strategies such as implantable loop recorders (ILR) are available and are being used more frequently. However, according to some authors, there is uncertainty about the benefit of implanting high-voltage devices in patients over 70 years of age to reduce their risk of mortality and improve their quality of life, given that there is insufficient representation of this population in the available clinical studies. 2
ILR have become valuable diagnostic tools for heart rhythm disorders that cannot be adequately recorded on a surface electrocardiogram or 24/48-hour Holter monitoring study. They have been proposed for patients who experience >1 episode every 15 days and patients with cryptogenic stroke under study for atrial fibrillation, showing a sensitivity of 100% and specificity up to 97%. They can also be used as complementary tools to electrophysiological test or head-up tilt table test in patients with a history of syncope. 3-6 Furthermore, these devices have been used to monitor older patients with frequent falls in whom the mechanism has not been established. 7,8
CASE PRESENTATION
An 87-year-old female self-reliant low-income patient from the rural area of Caldas, Colombia, attended consultation due to a fall without loss of consciousness in her home with transitory alteration of the language. There was no evidence of orthostatic hypotension on admission, and a history of hypertension and thyroid hormone replacement therapy was reported. The fall was interpreted as a neurological event: transient ischemic attack.
During a hospital stay, the patient presented normal ventricular function according to a transthoracic echocardiogram, brain scan without acute lesions, carotid Doppler without significant stenosis or unstable lesions, surface electrocardiogram in sinus rhythm, and 24-hour Holter study without evidence of atrial fibrillation, pauses or bradyarrhythmias. Implanting a heart monitor was proposed in order to find atrial fibrillation; the device was implanted in the fifth intercostal space at the left sternal border at a 45-degree angle under local anesthesia and percutaneously, without incisions or sutures.
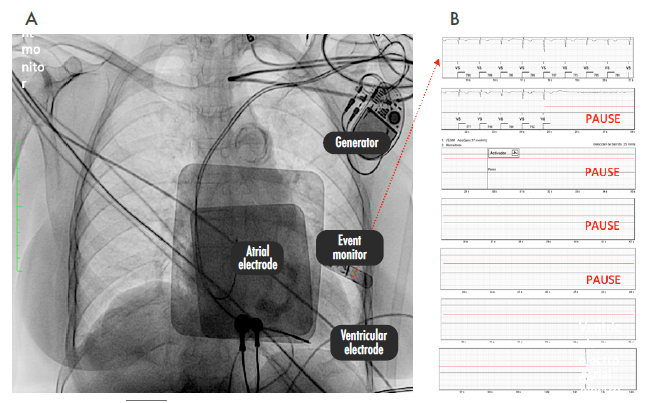
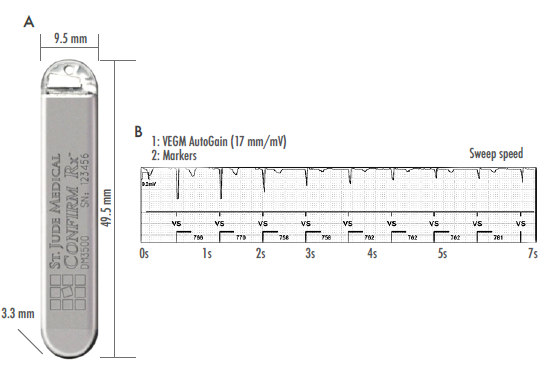
The first surgical follow-up visit took place 30 days after the procedure. The patient attended the appointment in the company of a granddaughter, who reported having activated the device due to multiple trips and falls without frank loss of postural tone. The data retrieved from the Confirm RX® device (St. Jude Medical, Figure 1) was analyzed and multiple sinus pauses were observed -the longest lasted 36 seconds-, so a new admission for a bicameral pacemaker implant was ordered. This procedure was performed by dissecting the cephalic vein with insertion of electrodes to the septal and apical region of the right ventricle and the right atrium; there were no complications (Figure 2).
Source: Document obtained during the study.
Figure 1: A) Insertable cardiac monitor Confirm Rx®; B) 7-second recording fragment recovered from the event monitor.
DISCUSSION
Up to 40% of strokes have no specific cause. However, this study found that monitoring using ILR was better than conventional tools to identify atrial fibrillation, the leading cause of stroke. 9
Fall episodes in older adults are common, dangerous and underestimated in some clinical settings. The highest frequency of falls is reported in patients over 80 years of age, with figures of up to 36%. 10 Therefore, establishing the correct cause of a fall is a clinical challenge considering that there may be one or multiple causes including dementia, gait abnormalities, weakness, sarcopenia, medications and arrhythmias (bradyarrhythmias and tachyarrhythmias). 10
When non-invasive diagnostic studies are performed, identifying sinus arrest as the cause of syncope is a challenging task; however, it can be recognized for being a long and sudden pause not preceded by a p wave and twice as long as the preceding P-P interval. Episodes of asystole, pulseless electrical activity, ventricular fibrillation and pulseless ventricular tachycardia are actually rhythms associated with cardiac arrest, so management requires adherence to cardiopulmonary resuscitation protocols. In countries such as the United States, estimates are that there are 290 000 cases of cardiac arrest every year, of which up to 88% are related to asystole or pulseless electrical activity. 11
The use of state-of-the-art percutaneously inserted ILR with minimal risk of infection (almost non-existent) allows identifying heart rhythm disorders in between 14% and 40% of cases related to recurrent falls of unknown origin. 12,13 Bhangu et al. 7 conducted a study using ILR in 70 patients aged 51-85 years with recurrent falls and syncope, and reported that the use of these devices allowed them to implant bicameral bradyarrhythmia pacemakers in 14% of cases and perform supraventricular tachycardia ablation in 4%. Moreover, the authors noted that ILR allowed them to recognize 71.4% of arrhythmia episodes and 20% of arrhythmias related to recurrent falls, identifying 8% of patients with bradycardia <40 bpm, 44% with bradycardia between 40 and 60 bpm, 30% with supraventricular tachycardia, and up to 18% with asystole >3 seconds. 7
Unexpected heart rhythm disorders in patients over 80 years of age are of clinical interest and radically change treatment behaviors. In this regard, some studies have reported cases in which diagnosis was achieved based on the analysis of ILR records, finding that up to 44% of syncopes of unknown cause were attributed to arrhythmias. This allows establishing specific treatments in order to reduce mortality, which in these patients is close to 32% at the time of diagnosis. 14-16
The benefit of using ILR has been widely studied. Ryan et al. 17 analyzed their utility in other types of pathologies such as carotid sinus hypersensitivity in fourth age patients by means of multicenter, double-blind and randomized designs in a limited sample; however they did not obtain conclusive results. On the other hand, Maggi et al.18 investigated their use in patients with non-syncopal loss of consciousness and found that ILR recorded asystole >6 seconds in 26% of the cases.
Based on the observations in this case report, ILR should be routinely used in older patients with unexplained falls, as this intervention allows elucidating heart rhythm disorders that can be treated and, thus, improve their quality of life. In the case of arrhythmias, the use of these devices would allow avoiding fatal outcomes and prolonged hospitalization stays due to repeated falls, as well as improving the day-to-day life of these patients.
One limitation of this study was the lack of other exploratory diagnostic studies, since they were not considered necessary by any of the specialties that treated the patient. However, it should be noted that although evidence on the use of ILR in people aged 80 years or above is limited and not conclusive, in this case the device was useful for the resolution of a problem frequently found in clinical practice.
CONCLUSIONS
Since recurrent falls and syncope have a multifactorial component, in older adults the presence of arrhythmias (bradyarrhythmias and asystole or tachyarrhythmias) should be considered as a possible cause of these events.
The use of diagnostic tools such as ILR allows the patients and their relatives to correlate the symptoms with the heart rhythm at the time of the event, which can help clinicians make appropriate and accurate decisions for the treatment of recurrent falls of cardiac origin or syncope of unknown cause in older people.