INTRODUCTION
The term arthrogryposis is derived from the Greek words "arthron" (joint) and "gryposis" (hooking). Arthrogryposis multiplex congenita (AMC) is a multifactorial and heterogeneous disorder characterized by non-progressive joint contractures involving at least two joints; this condition can be recognized at birth. 1
AMC has an estimated prevalence of 1 case per every 3 000-5 000 live births, with the same male-to-female ratio. There are multiple types of AMCs, and most of them have a genetic origin; likewise, there are isolated cases or cases derived from environmental causes. 2,3 The exact etiology of this disorder is not clear yet; however, it has been established that any situation, whether maternal or fetal, that leads to decreased fetal movement can produce contractures and progress to deformity. In view of the unusual nature of the pathology, this paper reports the case of a newborn with AMC who received multidisciplinary treatment and had an early and adequate outcome.
CASE PRESENTATION
Newborn male patient, from non-consanguineous parents, product of a second pregnancy with low obstetric risk, and with adequate prenatal care checkup appointments, who presented a lower limb deformity at birth. The mother was 27 years old, had a high school diploma, worked as a baker, was enrolled in a health promotion entity through the contributory scheme, lived in a middle-income household and had a history of ectopic pregnancy. She did not have gestational diabetes, nor TORCH infections (Table 1), and the ultrasound scans were normal and showed no data suggesting malformations.
Table 1 TORCH panel test results during pregnancy.
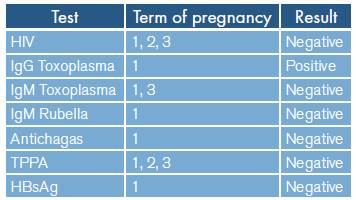
HIV: human immunodeficiency virus; IgG: immunoglobulin G; IgM: immunoglobulin M; HBsAg: Hepatitis B surface antigen; TPPA: Treponema pallidum particle agglutination test.
Source: Own elaboration.
At 35.6 weeks of pregnancy, as calculated by first trimester ultrasound measurement, the mother had a rupture of membranes for less than 18 hours, so she received antibiotic prophylaxis with ampicillin and labor was induced with oxytocin. The patient was born vaginally with cephalic presentation and difficult extraction that did not require using assisted vaginal delivery; he was transferred to the neonatal intensive care unit for neonatal resuscitation with supplementary oxygen.
Physical examination at birth found gestational age of 36 weeks according to Ballard's test, weight of 2 670gr (suitable for gestational age according to intergrowth), length of 49cm and head circumference of 31cm. A hyperextension deformity of the knees (passive flexion of 20° in the left leg and 30° in the right leg) was observed in the lower limbs, causing pain on movement (Figure 1). Similarly, retractile left testicle, adequate distal perfusion and symmetrical peripheral pulses of good intensity were documented. Ortolani and Barlow maneuvers were negative, and no midline injuries were evident. The patient was hospitalized with initial clinical suspicion of AMC; congenital knee dislocation was considered as a differential diagnosis.
During the hospital stay, a pelvis X-ray was of the femoral diaphysis and no ossification of taken, showing flattening and bilateral increase the proximal femoral nuclei; the morphology of in acetabular tilt angles with partial discovery the iliac wings was normal (Figure 2).

Source: Document obtained during the study.
Figure 2 Pelvis x-ray in newborn with hyperextension of the knees.
Given these results, a neurological examination was performed, and normal findings were observed. This suggested that this condition could be caused by either of the two main types of AMC: amyoplasia or distal arthrogryposis. 4
The patient was discharged at five days of life. Outpatient checkups included assessment by the pediatric neurology service, which requested auditory evoked potential test and electromyography of the four lower limbs that yielded normal results and reported no complications or adverse events. Similarly, the pediatric orthopedics service did a follow-up of the case and performed a dynamic ultrasound which ruled out congenital hip dislocation.
Physical therapy was indicated as the only treatment. Activities at home consisted of stretching each contracted joint in 2 repetitions of 30 seconds after the bath, when the baby was more relaxed or when the baby was being fed. The baby's neck had to be stretched in bilateral flexion and left rotation using toys or the parents' faces to get his attention and make him turn his head to the left; the patient evolved favorably. These exercises were also reinforced by using splints on the joints during naps and before the child fell asleep at night. Moreover, parents could also put the baby in supine position on their legs and then switch to prone position or emphasize the extension of the neck while sitting and leaning forward at the edge of the parents' knees. The parents were also informed about the possibility that their child could develop scoliosis due to decreased asymmetric muscle strength, stressing the importance of frequent spinal screening for the same reason. 5
At the time of writing this report, the patient had achieved almost full recovery of the motion of the arches in both hips and knees (Figure 3). This leads to think that his rehabilitation was easier because the somatopic arrangement in the cerebral cortex is less affected due to the isolated involvement of the lower limbs, as opposed to the typical presentation in the four limbs. The patient had a normal karyotype report and no further molecular studies were requested, nor was a muscle biopsy performed since his general condition improved.
DISCUSSION
AMC can be a manifestation of several neuromuscular diseases. 6 The main joints affected by this condition are the feet, knees, hips, waist and elbows, 7,8 and its etiology ranges from monogenic diseases to environmental factors that affect the mother or the fetus, including infections, drugs, oligohydramnios, trauma and structural abnormalities of the uterus. 9
Fetal movements are of great importance for the development of the joints and periarticular tissue since their absence can lead to fibrosis and joint contractures. 10,11 Regarding the latter aspect, it should be noted that the severity of the contractures is mainly determined by the moment in which they appear; thus, the most severe and disabling contractures will occur if movement decreases in the first months of gestational age. 4
Ultrasound monitoring during prenatal assessment can be a useful tool; 9 although its sensitivity for the detection of specific abnormalities requiring specialized care can range from 8.3% to 74.4%, its positive predictive value for major malformations is 90.4%. 12 At this point, it is important to mention that 75% of AMC cases are not diagnosed before birth because the ultrasonographic technique requires observing fetal movements for a long time and they are not evident until the 16th-18th week of gestation. 2,13 Diagnostic tests should examine the pulmonary and renal systems as some conditions may overlap with AMC due to sporadic, syndromic, neurogenic, myopathic, and metabolic causes. 13
As mentioned above, there are two types of AMC, namely, amyoplasia, or distal arthrogryposis, which have 10 different types based on the 2009 Bamshad classification; 2,14 (Table 2) amyoplasia is the most common form of AMC. It is not associated usually with genetic disorders, and is characterized by an atrophic muscle tissue that is replaced by fatty and fibrous tissue; in addition, it may involve all four limbs in a symmetrical pattern and the shoulders are generally rotated and adducted internally, the lower limbs and hips are dislocated, the knees are extended, and the feet are equinovarus (as in the present case). It should be noted that the case described here is atypical since it did not involve all four limbs but only the lower limbs.
Table 2 Classification of distal multiple congenital arthrogryposis according to Bamshad.
Source: Own elaboration based on Bamshad et al.14
Patients with suspected AMC and corpus callosum agenesis, lisencephaly, ventriculomegaly, microcephaly or cerebellar vermis aplasia require fetal MRI for the correct diagnosis of brain disease. 9 Similarly, in order to guide AMC classification, differential diagnosis and give advice to the family, a complete physical assessment should be performed at birth. It must include neurological and affected joint examination; identification of limb contractures (most frequent finding in AMC patients and found in 67% of cases diagnosed prenatally); 15 electrophysiological studies; muscle and nerve biopsy; and gene sequencing 3,7.
AMC is related to over 400 specific medical conditions and over 350 genes are involved in its development. 7 The majority (70-85%) of patients present with associated neurological alterations, which usually have a genetic origin with autosomal recessive, autosomal dominant or X-linked mechanisms of inheritance; however, there are a large number of cases that are sporadic or idiopathic. 7,15 Thus, given the wide variety of clinical presentations and the considerable number of triggering mutations, determining the primary cause of a specific type of AMC is a challenge.
The therapeutic approach to AMC is based on surgical reconstructions, orthopedic management, and physical and rehabilitative therapies for extended periods. 14) In this sense, it is important to know that the long-term prognosis of patients with this disease is favorable if there is an adequate multidisciplinary treatment that improves their quality of life. In this respect, Polania-Rodriguez et al.11 demonstrated that patients who receive adequate treatment have a normal level of intelligence and have a more independent life in adulthood.
The literature only has three similar case reports in which patients received care with a multidisciplinary approach for their rehabilitation and orthopedic treatment. 5,10,11 This led to rethinking other differential diagnoses that might be worth including to guide readers to similar findings.
In this case, it is noteworthy that the deformities did not involve all four limbs and, therefore, did not fully fit into any of the existing classifications. In addition, the patient presented a favorable clinical course. Consequently, it is important to consider that the patient's condition could also be explained by an isolated congenital dislocation of the knee, or by an AMC-associated dislocation. 16-18
Likewise, the patient presented with some clinical features compatible with the alternative diagnosis of congenital knee dislocation, such as joint instability, reduction of dislocation with snap or piston, muscle retraction (knee quadriceps, hip adductors), restricted range of motion (hip abduction) and presence of skin folds or grooves, 18 which were more noticeable after achieving complete improvement (Figure 3).
Congenital dislocation of the knee is a rare condition (1 case per 1 00 000 live births) 17 and is easily diagnosed in the first hours of life. Usually, physical examination is sufficient to observe the marked hyperextension of the knee in contrast to the habitual position in flexion, although a radiography can support the diagnosis. At this point, it is worth clarifying that knee involvement is common in AMC disorders, ranging from soft tissue contractures to subluxation and dislocation; specifically, knee problems can be found in up to 38-90% of amyoplasia cases. 19
The treatment for AMC and congenital knee dislocation is the same, and the recommendations for physical therapy described above should be maintained for 4-8 weeks; depending on the case, a splint and even surgery may be indicated if therapy fails. 16
CONCLUSIONS
Antenatal suspicion, thorough physical examination and differential diagnosis are of vital importance to achieve a satisfactory clinical course in AMC patients; this allows providing proper management, minimizing diagnostic errors, avoiding unnecessary procedures, and performing effective and timely treatment with outstanding results. It should be noted that for the optimal and accurate management of this condition, specialties such as pediatrics, orthopedics, physiatry, neurology and genetics should be involved.
















