INTRODUCTION
Pancreatic injury (PI) is rare but catastrophic and difficult to diagnose due to the retroperitoneal location of the pancreas and the fact that 90% of the cases are associated with an injury in other organs, mainly the duodenum, which can lead to an erroneous initial diagnostic approach. 37% of PI occur after receiving a blunt trauma, especially in the epigastric region, leading to the compression of the intra-abdominal organs against the spine and damaging the pancreas. The most common PI include acute bleeding, pancreatic pseudocysts, pancreatic abscesses, pancreatic fistulas, pancreatitis and, to a lesser extent, acute bleeding, and splenic vein thrombosis. 1-7
Traumatic pancreatitis (TP) comprises less than 10% of all abdominal traumas but can reach mortality and morbidity rates of up to 34% and 64%, respectively. The mechanism of injury, increased blood levels of the pancreatic enzymes and imaging findings in ultrasound and in computed tomography (CT) and computed axial tomography (CAT) scans must be taken into account for diagnostic purposes. At present, the treatment of PT is usually non-surgical, beginning with a conservative medical approach. If the expected outcomes are not achieved, the second option is using minimally invasive procedures such as endoscopic or percutaneous techniques; finally, surgery is considered if the evolution of the patient is torpid. 1-9 The following is a case report of a patient with PT who underwent laparoscopic surgery due to the poor response to watchful waiting, obtaining a satisfactory evolution.
CASE PRESENTATION
The following is the case of a 54-year-old male farmer from Yagura (Huila, Colombia), previously healthy and with no medical history, who was admitted to the emergency department of the Hospital Universitario Hernando Moncaleano Perdomo 4 hours after suffering a blunt trauma in the right hypochondrium due to a bovine kick. The man reported pain exacerbated by food intake. Physical examination showed the patient to be hemodynamically stable with soft abdomen, painful on palpation, no signs of peritoneal irritation and ecchymosis in the right hypochondrium.
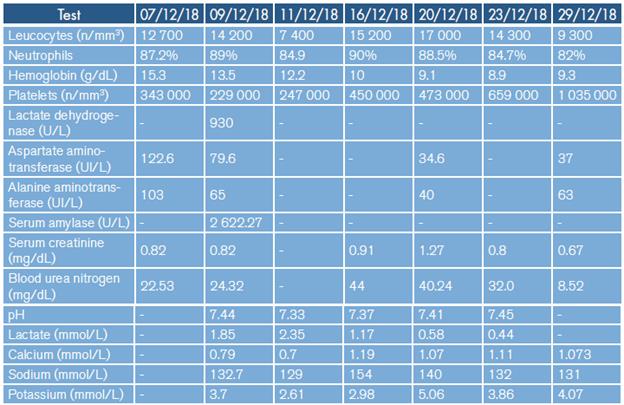
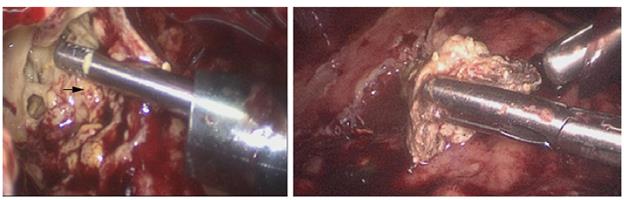
A focused assessment with sonography in trauma (FAST) scan was performed on admission, yielding negative results for intra-abdominal fluid. Laboratory tests showed mild leukocytosis, low hemoglobin levels that did not require transfusion and increased transaminases, without other alterations (Table 1). Due to the persistence of pain, a computerized axial tomography (CAT) scan with double contrast was ordered (Figure 1), which showed distended gallbladder, normal pancreas, scarce free fluid in the peritoneal cavity and increased mesenteric density. Since the presence of leukocytosis, decreased hemoglobin levels, elevated serum amylase, and acidemia persisted, the patient was considered to have a poor evolution.
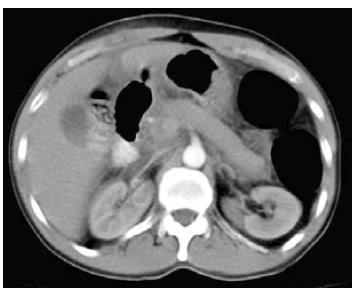
Considering the deterioration of the patient's condition and the persistence of pain, a serum amylase test was taken 72 hours after admission, obtaining a value of 2 622.27 U/L (25-125 U/L) that allowed diagnosing TP with a score of 2 according to the APACHE II system (mortality <4%) 10. 96 hours after admission, the patient presented emetic syndrome, diarrhea, abdominal distension and a 3.1 g/dL drop in hemoglobin levels. A second CAT scan was performed (Figure 2), revealing a laceration of 3mm in diameter at the head of the pancreas and increased free fluid in the peritoneal cavity, indicating a grade IV PI according to the Organ Injury Scale of the American Association for the Surgery of Trauma. 11
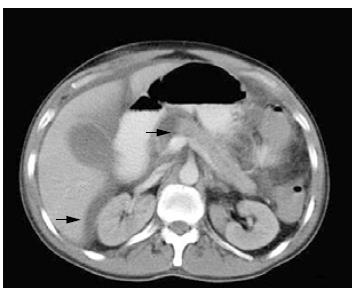
The patient's condition remained critical; for 2 more days he presented increased intra-abdominal pressure and abdominal pain, decreased urine output and intolerance to the oral route, so compartment syndrome was suspected, and an exploratory laparoscopy was performed. The following findings were observed: steatonecrosis in the parietal peritoneum and greater omentum with involvement of all the peritoneal cavity, multiple peritoneal adhesions from the greater omentum to the parietal peritoneum, 600cm3 of dark yellowish serosanguinous peritoneal fluid, thickened omentum and blood collection the transcavity of the omenta around the area of pancreatic injury, drained towards the peritoneal cavity with friable and inflammatory tissue that evidenced scarce bleeding of the traumatic fracture in the neck of the pancreas; no abnormalities were observed placed in the transcavity of the omentum and in in the other areas of the peritoneal cavity or in the left parietocolic gutters, which were attached the intraperitoneal structures. Two drains were to the skin (Figure 3).
Forty-eight hours after the surgery, the patient scored 13 points in the APACHE II classification (mortality between 11% and 18%). He also presented with metabolic acidosis, tachycardia, and tachypnea, and did not have an adequate modulation of the systemic inflammatory response. As a result, a new laparoscopic peritoneal lavage was performed, finding areas of generalized steatonecrosis with involvement of the entire peritoneal cavity, multiple rolling adhesions from the omentum to the parietal peritoneum,yellowish serosanguinous peritoneal fluid collection in transcavity, and yellowish se-rosanguinous peritoneal fluid of approximately 500cm3 in the peritoneal cavity. 10
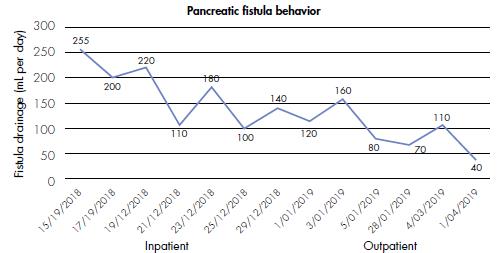
Following this procedure, the patient presented with acute respiratory distress syndrome, poor modulation of the inflammatory response and negative blood and peritoneal fluid cultures. Broad-spectrum antibiotic treatment (2g of cefepime) was started intravenously every 8 hours and low-output pancreatic fistula was considered after quantifying the drains, with an average of 1 37 mL/day and fluid amylase of 76 396 U/L (25-125 U/L) (Figure 4). 12
Finally, the patient was diagnosed with moderate-severe TP. Multidisciplinary management was indicated along with mixed nutritional support (enteral and parenteral for 3 days and total parenteral for 7 days) and antibiotic therapy for 19 days. The surgeries were performed on the fifth and eighth day of admission and two days after the patient was transferred to the intensive care unit where he stayed for 9 days; the patient spent the rest of his stay on the floor and was discharged from hospital 29 days after admission with an arranged low-output pancreatic fistula.
The patient was subsequently monitored on an outpatient basis with progressive assessment of pancreatic fistula output. He was also given medical treatment and nutritional support with a diet rich in low-medium chain triglycerides and fat restriction. Adherence to treatment was adequate and the pancreatic fistula decreased progressively until it closed spontaneously in the fifth month after surgery.
DISCUSSION
PI represents between 0.2% and 1.1% of all traumas and can present in various forms: pancreatic leak, abscesses, fistulas, TP, pancreatic pseudocysts (which are the most common manifestation), acute bleeding (which has the highest mortality) and other rare manifestations such as peritonitis, gastrointestinal bleeding and splenic vein thrombosis. 1-4,6-8,13,14
TP has high morbidity and mortality rates and its diagnostic approach should be guided by clinical suspicion and the mechanism of injury. In this regard, it should be suspected in patients with blunt abdominal trauma caused by falls, blows with bicycle handlebars but especially automobile accidents, which account for 75-85% of the causes of PT due to direct impact of seat belts on the umbilical region. The clinical presentation of TP is characterized by nausea, vomiting and generalized abdominal pain or epigastric pain irradiated to the back (50% of patients) that may improve by adopting a genupectoral position; in severe cases, it may present with abdominal distension or hypovolemic shock secondary to hemoperitoneum. 1,3-7,13,14
Abdominal examination to treat TP may yield false negative results on the initial assessment in up to 34% of cases. In our patient, localized pain in the right hypochondrium and diffuse abdominal pain on palpation did not suggest TP; however, this pathology could not be ruled out because of the exacerbated postprandial pain and the mechanism of injury. 1,3,4,13,14
The diagnosis of TP should be multidisciplinary and rule out other causes of acute abdomen such as perforated hollow viscus, hemoperitoneum or peritonitis, so it is important to perform conventional laboratory test (blood count, blood urea nitrogen, serum creatinine, coagulation tests, serum amylase and arterial gases), standing chest X-ray (to rule out pneumoperitoneum) and FAST ultrasound. It should be noted that the latter is not useful for identifying TP because its aim is to rule out the presence of free abdominal fluid in the hepatorenal, splenorenal, pelvic and pericardial spaces and not to observe the pancreas. 1-3,6-8,15
Another method for diagnosing TP is the CAT scan; however, it has a sensitivity of 4779% for PI, may be normal for up to 12 hours after trauma in 20-40% of patients, and its sensitivity for identifying lesions in the duct of Wirsung is 43%. For these reasons, magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) are preferred. This patient underwent two CAT scans: the first did not show relevant findings (Figure 1), while the second showed a fracture of the head of the pancreas, intraperitoneal free fluid and peri-pancreatic fluid (Figure 2), findings that have a sensitivity of 67-85% for TP. 1,3,4
Serum amylase has a sensitivity of 67-83% and a specificity of 85-98% for detecting TP. Nevertheless, to be useful for diagnosis, its levels in the tests must be three times above the upper normal limit of the laboratory; in the reported patient this enzyme was elevated almost 21 times. 1,4,5,16
The treatment of TP depends on several factors. If the FAST ultrasound shows hemodynamic instability and peritonitis, laparotomy is possible; if other organs are involved, the extent of the injury and the grade of TP (injury in the duct of Wirsung, parenchymal involvement and location of the trauma) must be considered. 1,3-8
In patients with hemodynamically stable TP, the treatment is conservative and imaging studies are conducted to assess the degree of the PI. Performing ERCP or MRI is recommended if there is a change in lab test results and findings suggestive of injury in the duct of Wirsung in the CAT scan; those studies have sensitivity and specificity close to 100% for this type of injury. It should be noted that ERCP has the advantage of being both a diagnostic and therapeutic tool since, in some cases, it allows placing a stent in the duct of Wirsung, thus achieving endoscopic management of the pancreatic fistula. 1-7,17,18
For TP grades I and II, conservative management is recommended because surgery is associated with greater morbidity from chronic pancreatitis, fistulas, pseudocyst formation and longer hospital stays. For grades III to V diagnosed by CAT scan, the first therapeutic option should be clinical management with fluid resuscitation and nutritional support, depending on the patient's clinical condition. If the condition keeps deteriorating, a surgery should be performed given the risk of increased morbidity and mortality.
In general, and regardless of the grade of the injury, the open surgical approach is recommended; however, in recent years, with the rise of minimally invasive procedures, ultrasound-guided percutaneous drainage and laparoscopic surgery have been proposed. There is a group of patients with chronic formation of pancreatic pseudocysts in which drainage could be performed endoscopically; this procedure reaches an efficiency close to 90% and a significant reduction in morbidity and mortality rates. 2-7,19,20
Since the patient had grade IV TP due to the fracture of the head of the pancreas (Figure 2), as well as abdominal distension and a decrease of 3.1 g/dL in hemoglobin levels in two days, he was taken to laparoscopic surgery with the objective of draining intraperitoneal abscesses and doing a peritoneal lavage to reduce the local intra-abdominal inflammatory response. Few reports describe the laparoscopic approach to acute pancreatitis, as it is more common in patients with necrotizing pancreatitis who undergo pancreatic necrosectomy, 1-7,9,19,20 condition that can be treated using the retroperitoneal or the transperitoneal approach.
Both techniques differ in terms of the anatomical site involved. Their advantages and disadvantages are presented below: 21-23
The retroperitoneal surgical approach has less risk of peritoneal contamination, but the type of access and the visualization of the pancreas that it allows limit the amount of detritus removed, so reinterventions may be needed to control infectious processes. This technique has a success, morbidity, and mortality rate of 64%, 47% and 14%, respectively. 21-23
The transperitoneal surgical approach has the advantage of controlling the retroperitoneal and intraperitoneal spaces, which allows draining blood collections, exploring the omental pouch and performing peritoneal lavage, formal pancreatic necrosectomy and partial or total pancreatectomy; because of its wide field of vision and maneuverability, only one intervention is necessary to achieve a complete pancreatic necrosectomy. Among the disadvantages of this approach are the contamination of the intraperitoneal space and the difficulty of reintervention due to increased development of peritoneal adhesions. 21-23) In the present case, due to the imaging findings and the presence of free intraperitoneal fluid, the transperitoneal surgical approach was selected. During the second surgery, blood collections were controlled, and the pancreatic fistula was satisfactorily arranged, obtaining a favorable outcome. To achieve the patient's improvement, a multidisciplinary outpatient management guided by general surgery, clinical nutrition and physiotherapy was performed, with which the fistula output was progressively reduced, with its subsequent closure, while the patient's nutritional status improved.
CONCLUSIONS
TP diagnosis is challenging due to the retroperitoneal location of the pancreas. The treatment is usually conservative and watchful waiting and percutaneous or endoscopic drains are preferred over surgery. The recommended surgical approach is laparotomy, although the laparoscopic approach may be a good option to treat this pathology.