INTRODUCTION
Spontaneous pulmonary herniation (SPH) is a protrusion of the lung into an abnormal opening through the parietal pleura that occurs at the level of the chest wall, diaphragm, or mediastinum 1. It can be caused by costal arch fractures without a history of trauma. It has also been reported in cases of chronic coughing patients 2. SPH is a rare entity and only about 300 cases have been reported worldwide 3.
According to its etiology, Morel-Lavallée 4 classified pulmonary hernias as congenital or acquired; in turn, the latter are classified into spontaneous or caused by local and traumatic diseases.
SPHs are usually located at the intercostal space and associated with previous thoracic surgeries, particularly thoracotomies 5,6, or chest trauma 7. SPHs are the least common form of pulmonary hernia, and there are few records of them presenting during a coughing or sneezing episode 8.
SPH is diagnosed primarily based on clinical symptoms such as chest pain and dyspnea, as well as a hernia defect that can be large and mobilized with Valsalva maneuvers and respiratory movements 9. The diagnosis is usually confirmed by an oblique chest x-ray or a non-contrast chest computed tomography (CT) scan in its different planes 10.
While surgery is the most common treatment for SPH, conservative management is still under debate. It should be noted that there is no standard surgical technique to treat this type of protrusion. However, surgery 11 is indicated to treat the defect with primary closure either by using autologous tissue; synthetic materials such as Teflon, dacron, ivalon, GoreTex® 12 or Marlex®; or osteosynthesis materials designed specifically for the chest wall, such as wire and transcostal sutures, Kirschner wires or pins, metal plates (Judet struts) and titanium plates 7-13. Jheon S et al.14 reported correction by means of videothoracoscopy.
The following is the first case of SLH reported in Ecuador.
CASE PRESENTATION
A 59-year-old male patient, Hispanic, from Guayaquil (Ecuador), an office worker, from a middle-income family, hypertensive, with diabetes under control and no history of surgery, trauma or inherited disease, attended the emergency department of the Hospital Clínica San Francisco of Guayaquil due to a 3-day history of hemoptysis, moderate pain in the right hemithorax, and subsequent appearance of edema and a small hematoma at the right submammary level. He also presented with a hernial defect of the thoracic wall that was noticeable during respiratory movements and the Valsalva maneuver (Figure 1). The patient was able to breathe without supplemental oxygen and his vital signs were stable.
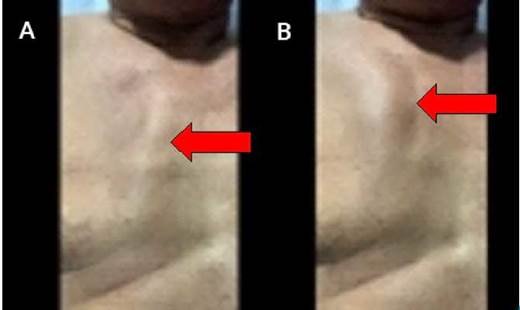
Source: Document obtained during the course of the study.
Figure 1 Patient morphology. A) Right parasternal depression during inspiration; B) Pulmonary hernia during Valsalva maneuver.
On admission, laboratory tests showed leukocytosis of 15.55x103/uL with 75.4% neutrophilia; all other tests were within normal values. Anteroposterior chest x-ray showed accentuation of bilateral pulmonary interstitium, pleural effusion, and obliteration of right costophrenic and cardio-phrenic angles. Pleural ultrasound revealed right pleural cavity with fluid (approximate volume: 1 061cc with no septa or sediment) and collapse of lower segments with air bronchogram in the right lower lobe.
Moreover, a non-contrast CT of the chest showed free fluid in the right pleural cavity of the aortopulmonary window (Figure 2), alveolar infiltrate in a diffuse distribution patch in the anterior segment of the right upper lobe, protrusion of the medial segment of the middle lobe and alveolar infiltrate in posterior segments of the right lower lobe, thus indicating the presence of pulmonary parenchyma outside the right pleuropulmonary cavity. On the other hand, a three-dimensional computed tomography reconstruction showed displaced ribs fracture (2nd to 5th rib) in the right hemithorax with collapse next to the median plane in the bony window (Figure 3). Based on these findings, a middle lobe pulmonary herniation with an alveolar pattern was suspected, with possible association with the area of pulmonary contusion, right pleural effusion, multiple costal fractures in right hemithorax and community-acquired pneumonia (CAP).
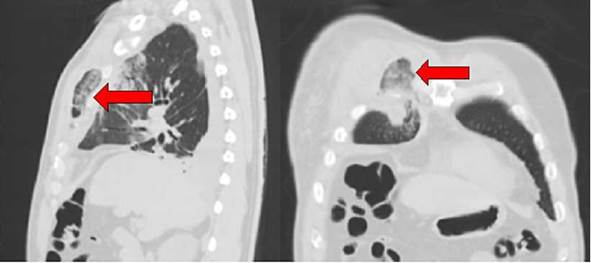
Source: Document obtained during the course of the study.
Figure 2 Non-contrast CT of the chest, sagittal and coronal planes.
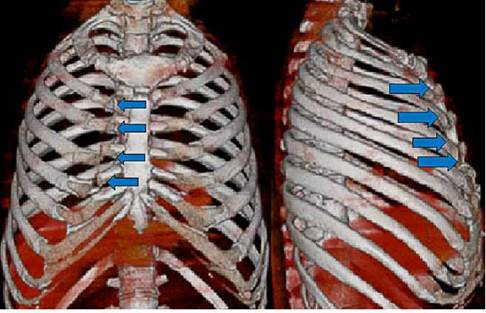
Source: Document obtained during the course of the study.
Figure 3 3D computed tomography reconstruction of the chest, coronal, and sagittal planes.
Blunt chest trauma and costochondritis were suggested as potential differential diagnoses for this case; however, the patient did not experience any current or previous trauma or chronic pain at the fracture site, so these diagnoses were ruled out.
When the patient was admitted to the emergency department, thoracentesis was also performed placing a 28Fr chest tube on the right side connected to the chest drainage system (Thorametrix™). During this procedure, a culture of the fluid was taken, which showed no evidence of bacterial growth and the biochemical study showed exudate according to Light's criteria.
The patient was admitted to the intensive care unit (ICU) after a few hours and was treated for CAP with 1.5g of ampicillin/sulbactam IV every 6 hours for 4 days and 500mg of clarithromycin IV every 12 hours for 7 days. The pulmonology service in the hospital ward decided to switch to intravenous meropenem 1g every 8 hours for 7 days due to the occurrence of fever no higher than 38°C and leukocytosis with no apparent focus other than pulmonary.
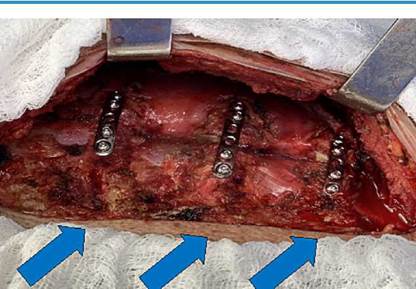
After 11 days of hospital stay, due to clinical improvement, the hernial defect was repaired by right thoracotomy with a parasternal incision of ±10cm. A hernial defect was found with protruding pulmonary parenchyma (Figure 4) through displaced fractures in the 2nd, 3rd, 4th, and 5th ribs of the right hemithorax. Similarly, reduction of herniated pulmonary parenchyma was performed and deperiostization and osteosynthesis were performed with miniplates and titanium screws between the 3rd and 5th ribs, fixing them to the costochondral junction (Figure 5). Thorametrix™ chest drainage was not removed. This surgery, which lasted 120 minutes, ended without complications and the drainage was removed at 48 hours.
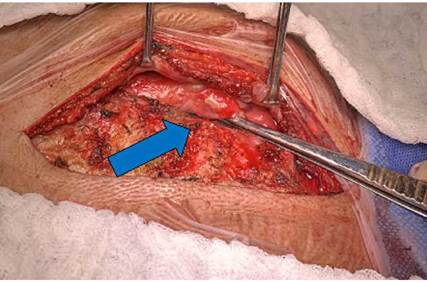
Source: Document obtained during the course of the study.
Figure 4 Hernial defect with protruded lung parenchyma.
Source: Document obtained during the course of the study.
Figure 5 Osteosynthesis material placed at the level of fractures in the 3rd, 4th, and 5th right ribs.
The patient remained hospitalized for 32 days (4 days in the ICU) and his stay was prolonged due to CAP and persistent leukocytosis. Five days after the surgery, he was discharged from the hospital and follow-up in the outpatient clinic was ordered.
At the time of writing this report, and three months after the surgery, the patient had a satisfactory recovery and was asymptomatic. Follow-up imaging showed correct placement of osteosynthesis material, but he was still monitored by a multidisciplinary team on a regular basis.
DISCUSSION
In Latin America, only one case of SHP was reported in Colombia in 2015, which was solved by video-assisted thoracic surgery (VATS) using a polypropylene mesh 14. Other publications have only reported intercostal or transdiaphragmatic hernias involving abdominal cavity structures 15,16, which are normally the result of thoracoabdominal trauma 17 and are treated with open surgery and prosthetic materials.
Worldwide, reports on SHP are also scarce: Nielsen & Nielsen 18 published a single case in 1971 and Cantó et al.19 presented 7 cases of costal fractures in 1985, of which only 4 had pulmonary herniation, indicating their rarity.
Other authors, such as Mitchell 20, Derbes & Haran 21, Wynn-Williams 22) and Pearson 2, identified pulmonary herniations in tuberculous or chronic bronchitis patients and reported that they were caused by the patients' effort due to repeated coughing. Kronenberger 23, on the other hand, addressed some costal fractures that he referred to as spontaneous, but he did not specify their etiology.
As mentioned above, pulmonary hernias may be congenital or acquired. The former are caused by the weakness of the suprapleural membrane are located in the cervical thorax between the scalene and sternocleidomastoid muscles, and can be seen with Valsalva maneuvers; they are also asymptomatic and disappear with growth. On the other hand, the latter are usually post-traumatic 7 or postoperative due to failure of surgical closure of the thoracic wall, most often after thoracotomies 5-6, but they may also be attributed to malignant neoplasms (metastasis) and, less commonly, cough 24.
It is worth noting that attempts have been made on multiple occasions to link cough to rib fractures as a result of prior conditions such as osteoporosis and senility, which is highly debatable considering that cases have also been reported in young patients 25. According to Pearson 2, the key factor for determining chest wall weakness is anterior serratus muscle tension for the first 8 ribs and external oblique tension for ribs 6 through 12. Additionally, and under this same concept, Jacka & Luison 11 state that rib fractures may be related to 3 factors: physical constitution, abdominal plethora, and cough in chronic bronchial patients.
SPH was found in the right hemithorax between the 2nd and 5th ribs in this case; however, several authors 7,10-11 claim that they occur more frequently in the left hemithorax and between the 8th and 9th ribs. The involvement of the liver, an organ that prevents the ipsilateral hemidiaphragm from abruptly shifting, is an anatomical reason for the rarity of this form of hernia on the right side. In the case series of Cantó et al.19, of the 7 patients reported, 6 had costal fractures in the anterior hemithorax, as in the patient reported here, and only 1 in the posterior hemithorax.
As in the present case, rib fractures and/or pulmonary hernias are usually accompanied by large hematomas in the thorax that extend to the abdomen. In some patients, pulmonary hernias are the consequence of a previous thoracotomy after receiving mechanical ventilation since the intercostal muscle is weakened by increased intrathoracic pressure with positive pressure 26. It should be noted that lung protrusion is more common in less extensive surgical procedures such as VATS because the form of closure is less meticulous 9.
An anteroposterior chest x-ray usually shows subtle, non-confirmatory changes such as radiopaque lesions similar to an alveolar infiltrate or areas of apparent lung contusion. If SPH is suspected, a non-contrast 3D CT scan reconstruction of the chest should be requested to confirm and identify the anatomy of herniation and determine whether herniation depends on a hernial sac or if it is accompanied by costal fractures. Likewise, it is important to establish early if there are findings of strangulation that require urgent intervention. Moreover, according to Clark et al.27, some herniations show up very clearly on coronal and sagittal CT planes, giving an overview of the area and extent of the disease and aiding surgical planning.
Regarding the treatment of SPH, there is still debate between conservative and surgical management. In the first case, immobilizing bandages are placed expecting the spontaneous closure of the hernia, provided that it is a minor lesion with mild symptoms; however, some of these patients have COPD and are unable to withstand the bandage.
The decision to opt for surgical treatment is related to clinical findings, recurrence of symptoms (particularly pain), and the presence of chest wall infection or incarceration 10. Surgery is thus indicated to treat the chest wall defect, and sometimes the hernial sac and non-viable tissue must be removed from the herniated lung 11,28.
Other authors report that SPHs can be corrected by video-thoracoscopy 14, although this is not a well-established technique. In the case presented here, there was no need to remove any part of the lung, as there were no drawbacks at the time of reducing the hernia manually and the chest wall defect was corrected without any further problem. Reduction of the pulmonary parenchyma should be considered if there is a possibility of any complication due to pulmonary hypertension or its recurrence. In the present case, since there was a chest wall defect with fractures at the costochondral junction, it was decided to place osteosynthesis material that had both ends of the bone and the sternum as support planes.
CONCLUSIONS
SPH is a rare disorder with a mostly clinical diagnosis that includes pain, involvement of a hernial defect, and a history of cough, although the latter is unusual. Currently, the diagnosis can be made with great accuracy, and the extent of the hernia and pulmonary involvement can be determined, allowing for surgical care.
Although the treatment for SPH has not been yet established, surgery is the most effective treatment choice due to the rapid improvement of the patient's symptoms and the prevention of recurrence. According to the few studies available on this condition, surgery may be done using an open or a video-assisted approach (none of which is yet protocolized), or even a combination of both approaches, especially if there are rib fractures.
The case presented here is relevant because it demonstrates that the surgical method using miniplate osteosynthesis and titanium screws can achieve optimal results, prevent recurrences, and fully alleviate symptoms. Therefore, this approach may be considered a viable option for the surgical treatment of SPH.














