INTRODUCTION
Heterotopic pregnancy is defined as the coexistence of an intrauterine pregnancy and an ectopic pregnancy at any location, although most cases occur in the uterine tubes 1. According to Zatarain-Gulmar & Torres-Hernández 2, the first case of heterotopic pregnancy was described by Duberney in 1708 in the findings of an autopsy.
Even though this type of pregnancy is extremely rare, it is estimated to occur in 1 out of every 30 000 to 50 000 spontaneous pregnancies. In recent years, there has been an increase in cases related to the use of assisted reproductive technologies since the prevalence rate increases by up to 1% in pregnancies achieved using these techniques 3.
Determination of the human chorionic gonadotropin ß-core fragment and transvaginal ultrasound are the most useful options for diagnosing heterotopic pregnancy. Methotrexate, hypertonic injectables, expectant management, and laparoscopic surgery are all options for treating this illness 4 and the best option should be chosen based on the expertise of the treating physician and the patient's clinical and hemodynamic status 5.
Heterotopic pregnancy is associated with high maternal morbidity and mortality, so its diagnosis and timely care are crucial. The following is the case of a patient who presented with abdominal pain suggestive of the aforementioned condition.
CASE PRESENTATION
A 32-year-old mestizo patient from the city of Pasto, Colombia, who worked as a nursing assistant and came from a middle-income household, consulted the emergency department of a tertiary health care institution. For five hours, she presented with diffuse, abdominal, colicky pain with predominance in the hypogastrium and right iliac fossa of moderate intensity that progressed to intense, associated with moderate vaginal bleeding. At the time of consultation, the patient was 5.1 weeks pregnant. She stated that it was his first pregnancy and that it was not the result of fertilization techniques. Her medical history revealed that she had hypothyroidism treated with levothyroxine 50mcg and that she had no surgical or allergy history and no sexually transmitted diseases.
On physical examination, the following vital signs were found: blood pressure of 120/80 mmHg; heart rate of 62 bpm; respiratory rate of 19 rpm; and temperature of 36.2°C. She also presented painful expression and soft abdomen, depressible and tender to palpation at the level of hypogastrium and right iliac fossa. Vaginal examination showed a closed central cervix and scant red vaginal bleeding, although no signs of peritoneal irritation were found.
In view of the findings, complementary laboratory tests were performed, showing C-reactive protein level of 0.57 mg/L; blood count with leukocytes of 16.85 mg/L, neutrophils of 90.4%, hemoglobin of 14.8 mg/L, hematocrit of 43.2%, and platelets of 294 mg/L; normal urinalysis; negative gram stain of uncentrifuged urine; and quantitative human chorionic gonadotropin ß-subunit levels of 16 627.77 mlU/mL.
Because gonadotropin levels were elevated for gestational age and the patient had vaginal bleeding, it was decided to perform a transvaginal ultrasound that showed anteverted retroflexed uterus with a well implanted gestational sac in the uterine cavity and adequate decidual reaction. In the right adnexa, an echogenic yolk sac of 47x29mm was observed, which is characteristic of the "tubal ring sign" or "bagel sign." The ultrasound reading concluded intrauterine pregnancy of less than 6 weeks and the presence of a right adnexal mass that ruled out a second extrauterine gestational sac with free fluid in the posterior sac fundus (Figure 1).
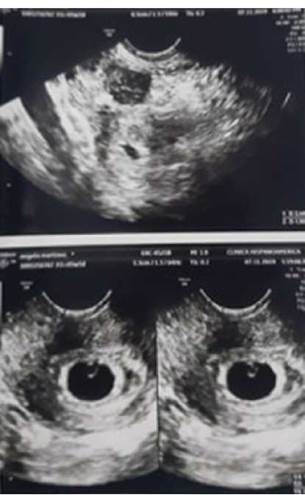
Source: Document obtained during the course of the study.
Figure 1 Transvaginal ultrasound with visualization of intrauterine pregnancy less than 6 weeks and right adnexal mass.
Due to the suspicion of heterotopic pregnancy, the patient was taken to laparotomy, a procedure in which there were no complications. A hemoperitoneum of 150cm3 was found and an ectopic right tubal pregnancy was confirmed, leading to a total right salpingectomy (Figure 2).

Source: Document obtained during the course of the study.
Figure 2 Sample removed during salpingectomy.
The patient progressed satisfactorily and was discharged with an indication for outpatient follow-up at 8 days, when a new transvaginal obstetric ultrasound was performed. It showed early pregnancy with retrochorial hematoma and a single live fetus that, according to fetal biometry, had a gestational age of 6.4 weeks.
At 12 weeks of gestation, the patient underwent a genetic screening ultrasound in which markers suggestive of chromosomopathy were detected, so she decided to request the voluntary interruption of her pregnancy.
DISCUSSION
Ectopic pregnancy is a serious public health concern in Colombia as it is one of the leading causes of maternal death. It is defined as the implantation of the blastocyst anywhere outside the uterine cavity 6,7, the most common location being the uterine tubes, with an incidence between 95 and 98%. Other less frequent locations are the cervix, ovaries, and abdomen 8-10.
Heterotopic pregnancy, on the other hand, is defined as the coexistence of a uterine and ectopic pregnancy 11. The literature reports that the main risk factors for this type of pregnancy are anatomical alterations of the uterine tubes, which in turn could be caused by infections; a history of pelvic inflammatory disease, tubal procedures, and ectopic pregnancy; use of intrauterine devices; and use of assisted reproductive techniques 12-16. However, in some cases, as in the case reported here, there is no associated risk factor.
The diagnosis of heterotopic pregnancy is based on clinical suspicion, but it should be confirmed with an ultrasound, preferably transvaginal, and the measurement of human chorionic gonadotropin levels. Ultrasound aids in the detection of significant findings such as an adnexal mass separated from the ovary, the tubal ring sign 17, and the visualization of another intrauterine embryo. It also helps to determine whether there is embryonic cardiac activity outside the uterus 18.
The ability to detect a heterotopic pregnancy in a timely manner is critical because it allows for the early adoption of appropriate treatment and, in this way, reduce maternal morbidity and mortality associated with this cause 19.
Although the symptomatology of heterotopic pregnancies may vary greatly depending on the location and weeks of gestation, the most common symptoms and signs include abdominal pain (80%), vaginal bleeding (50%), and hypovolemic shock (13%) 20.
There are several therapeutic options for treating this condition, including expectant management, medical management, and surgical management. Treatment with methotrexate and injection of hypertonic solutions in the extrauterine embryo are two options that are not currently recommended because their effects on intrauterine pregnancy are still unclear 21,22, which is why these options were ruled out in this case.
With regard to surgical treatment, laparotomy or laparoscopy may be performed, but the latter is chosen if the patient is hemodynamically stable and if the size of the ectopic pregnancy is adequate, because it is a safe technique and less painful and costly than the open surgical approach 23-25. In the clinical case presented here, laparotomy was chosen due to the presence of free fluid in the cul-de-sac, suggesting hemoperitoneum secondary to ectopic pregnancy that was confirmed during the procedure.
CONCLUSIONS
Although heterotopic pregnancy is a rare condition, it is an important cause of maternal morbidity and mortality. For this reason, it is essential that physicians are aware of it so that they can make a timely diagnosis and implement appropriate treatment. It should also be noted that this condition can have various clinical presentations.
Moreover, clinical signs and symptoms, human chorionic gonadotropin levels and ultrasound findings should be correlated in order to confirm a case of heterotopic pregnancy; it should also be considered that the pathognomonic sign of ectopic pregnancy is the visualization of the tubal ring sign and heterotopic pregnancy on ultrasound, as well as the visualization of intrauterine and extrauterine embryonic cardiac activity at the same time.
Finally, in cases of tubal ectopic pregnancies, medical treatment is not recommended as there is no evidence that intrauterine pregnancy may or may not be affected. As for surgical management, laparoscopy is the treatment of choice, as long as the patient's condition allows it.














