INTRODUCTION
Spermatic vein thrombosis (SVT) is a rare condition with a low clinical prevalence and no specific epidemiological data available due to a lack of published studies. The bibliography on this condition consists mainly of case reports, of which roughly 25 can be found around the world. Among the cases reported, it is evident that left lateral presentation is more common, which is explained by the anatomical variation in the drainage of the pampiniform plexus 1.
Thrombosis of the pampiniform plexus was first described in 1935 by McGavin 2; then, in 1950, Mathis & Claret 3 described spontaneous phlebothrombosis of the spermatic plexus; in 1970, Delevett & Goodrich 4 made the first SVT report; and in 1980, Coolsaet & Weinberg 5 reported three cases of this condition in children.
The treatment of SVT is conservative and includes the administration of anticoagulants at therapeutic doses, analgesia, local therapy, testicular suspension, and rest 1. Since it is a rare condition, understanding its main characteristics is critical to suspect it and provide the patient with timely treatment to avoid unfavorable outcomes. The following is the first case of this kind reported in Colombia and one of the few of the right laterality in the world.
CASE DESCRIPTION
A 21-year-old man from Bogotá D.C., Colombia, a university student, from a middle-class household and a medical history of mild traumatic brain injury without sequelae at the age of 20, was admitted to the Emergency Department of the Hospital Universitario Nacional de Colombia (a tertiary care institution) referred from another tertiary care hospital due to pain in the right inguinoscrotal region for a week, which progressively increased in intensity and exacerbated reaching a value of 8/10 on the analog pain scale. The patient also reported unquantified fever on one occasion and denied associated urinary symptoms or recent trauma to the scrotal region.
On physical examination upon admission, he was stable, with a soft abdomen, no signs of systemic inflammatory response and vital signs within normal limits. It was possible to establish that he had pain on deep palpation in the right spermatic cord, without palpable or visible varicocele and no signs of local infection, inflammation, or peritoneal irritation in the right inguinal canal. No inguinal hernias were observed, and the penis and testes were normal. No additional relevant findings were found in the other systems.
Initially, a testicular Doppler ultrasound was requested, which reported a non-compressible hypoechoic venous structure with thickened walls, located in the spermatic cord, extending into the pelvic cavity and compatible with right SVT. Furthermore, the study revealed inflammatory changes in spermatic cord fat that did not form abscesses or hematomas. It was found that the testes had well-defined contours, the epididymides were symmetrical, and the pampiniform plexuses had normal diameters. There were no signs of a cystic or solid focal lesion inside the testes and epididymides, and both showed normal echogenicity (Figure 1).
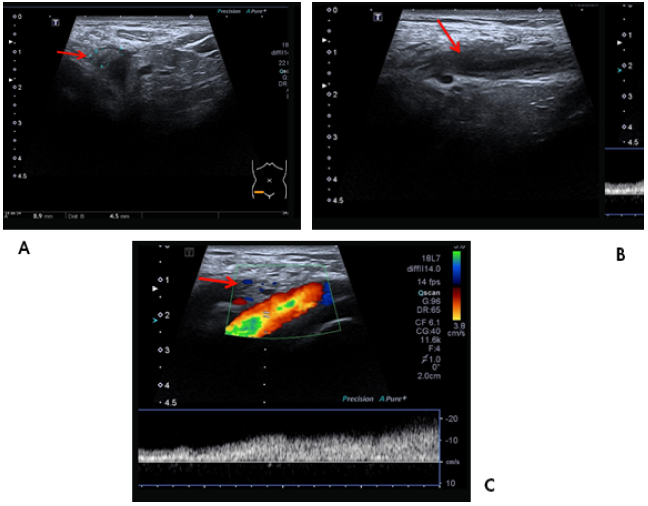
Source: Document obtained during the study.
Figure 1 Ultrasound study. A) right spermatic vein thrombus (arrow); B) longitudinal view of right spermatic vein with intraluminal thrombus (arrow); C) Doppler analysis showing disturbance of venous flow at the thrombus site in the spermatic vein (arrow).
Based on the ultrasound findings, laboratory tests were requested. The only relevant finding was a slightly positive C-reactive protein test (Table 1). With these results, and given the diagnostic impression, conservative treatment was immediately started with analgesia optimization (1g of intravenous dipyrone every 8 hours), full-dose anticoagulation with low molecular weight heparin (60 mg of subcutaneous enoxaparin every 12 hours), and local therapy.
Table 1 Laboratory tests.
| Study | Upon admission | Follow-up at 96 hours |
|---|---|---|
| Blood count | Leukocytes 7920 mm3 Neutrophils 49% Hemoglobin 16.4 mg/d Hematocrit 47.8% Platelets 211 000 mm3 | Leukocytes 7830 mm3 Neutrophils 41.1% Hemoglobin 15.4 mg/d Hematocrit 44.8% Platelets 258 000 mm3 |
| Clotting times | PT: 15.6 s INR: 1.161 PTT: 29.9 s | PT: 15.6 s INR: 1.16 PTT: 33.8 s |
| Acute phase reactants | CRP 19.56 |
PT: prothrombin time; PTT: partial thromboplastin time; INR: international normalized ratio; CRP: C-reactive protein.
Source: Own elaboration.
Furthermore, given the inflammatory findings at the right spermatic cord described in the ultrasound, the day after admission, it was decided to initiate an antibiotic regimen with norfloxacin 400mg orally every 12 hours and doxycycline 100mg orally every 12 hours for 10 days, after taking urine culture, which was negative.
On the second day of hospitalization, an assessment by the hematology service was requested, which ruled out systemic thrombotic disorders and considered that it was a right SVT possibly associated with deferentitis. Due to the risk of venous infarction, hematology also suggested starting anticoagulation with 60mg of subcutaneous enoxaparin every 12 hours until the international normalized ratio was therapeutic for 48 hours, and 5mg of oral warfarin every day until the ratio was maintained between 2 and 3 for three months.
The patient was discharged after five days and returned three months later for an outpatient follow-up appointment, during which a satisfactory clinical course was observed, with thrombus disappearance and complete relief of symptoms. No ultrasound follow-up images are available.
During hospitalization and discharge, the patient had a satisfactory evolution thanks to adequate tolerance and adherence to medical treatment, which did not generate adverse reactions. In addition, the man had no signs of systemic inflammatory response or infectious deterioration, and hemodynamic stability and pain resolution were achieved.
DISCUSSION
The etiology of SVT has not been determined because most cases occur spontaneously. Nonetheless, clinical conditions associated with the presentation of this disorder have been described, leading to the development of different theories about its possible origin. Authors such as Esmon 6, Grainge et al.7 and Murthy et al.8 have suggested that inflammatory bowel diseases, mainly ulcerative colitis and terminal ileitis, are possible causes of SVT since they are characterized by a prothrombotic state secondary to their inflammatory nature. Caño-Velasco et al.1, Bolat et al.9 and Diana et al.10 have also stated that hematological disorders, such as Henoch-Schönlein purpura or heterozygous factor V Leiden mutation and the use of psychoactive substances, such as cocaine, produce hypercoagulability states that can trigger SVT.
Other risk factors for venous thromboembolism such as cancer, hospitalization, recent surgeries, infections, trauma, inflammatory diseases and personal or family history of venous thromboembolism may also influence the development of SVT 11. In the reported case, it is suspected that the thrombus formed as a result of an inflammatory process in the ductus deferens; however, the cause of the deferentitis observed in the ultrasound is unknown.
Among the mechanical causes, it has been hypothesized that vigorous physical exercise, weight-lifting and abdominal trauma generate an increase in intra-abdominal pressure, which, in turn, increases venous pressure and, in addition to a decreased blood flow in the gonadal system, predisposes to the formation of thrombi 8,12,13. Nutcracker syndrome (increased pressure of the left renal vein secondary to compression by the superior mesenteric artery and aorta) and having undergone laparoscopic inguinal herniorrhaphy have also been associated with the development of SVT 14-16.
In addition, it is important to note that the anatomical connection between the testicular vein and the left renal vein allows kidney disorders, including neoplasms, to spread to the left spermatic vein and cause thrombosis. SVT has also been linked to renal, testicular, adrenal, gastrointestinal, hematologic, and liposarcoma cancers in that order of occurrence 11,17.
The frequent involvement of the left spermatic vein in SVT has been attributed to predisposing anatomical factors similar to those of varicocele formation or thrombosis of the left pampiniform plexus: the right testicular vein drains into the vena cava obliquely, while the left testicular vein drains into the left renal vein perpendicularly, resulting in increased left vein pressure and reduced ipsilateral flow 11.
The symptoms of SVT are non-specific, with the main clinical manifestations being: testicular pain, groin pain with or without irradiation to the scrotum or lumbar region, abdominal pain or discomfort, palpable masses in the inguinal canal or scrotum, edema or local erythema, fever, vegetative symptoms and macroscopic hematuria; all these symptoms exacerbate when patients are standing upright and perform Valsalva maneuvers and decrease with rest. Physical examination shows signs such as increased consistency and size of the spermatic cord, local inflammation, among others 1,18,19.
Due to the high variability and low specificity of symptoms, its clinical similarity with other conditions and its low incidence, a high suspicion rate is required to diagnose SVT. In this scenario, the occurrence of this event should be confirmed by radiological findings; however, it is important to keep in mind that surgical exploration is sometimes also necessary given the impossibility of distinguishing between incarcerated inguinal hernias or testicular thrombosis 19,20.
Doppler ultrasound is the gold standard test for the diagnosis of SVT due to its high sensitivity and specificity, compared to techniques such as angiography, its low cost and because it is a non-invasive method. However, CT angiography may sometimes be necessary to evaluate the extent of the thrombus 18,21. The findings of SVT on ultrasound include a hypoechoic image with absence of venous flow in the Doppler analysis at the level of the occlusion generated by the thrombus and a negative response to Valsalva maneuvers, which helps to differentiate it from varicocele 1,18.
The differential diagnosis of SVT includes testicular torsion, torsion of the appendix testis, epididymitis, orchitis, testicular trauma, idiopathic testicular infarction, incarcerated inguinal hernia, hydrocele, spermatocele, abscesses, thromboangiitis obliterans, and tumors 1,17,19.
There is insufficient information to provide evidence-based therapy recommendations for SVT because conservative management is recommended even though patients typically require surgery. However, Mallat et al.14 state that when the lesion is located outside the external inguinal ring (pampiniform plexus), conservative treatment could be selected, including anticoagulation associated with non-steroidal anti-inflammatory drugs, local therapy (ice and testicular suspension), and rest.
Likewise, Caño-Velasco et al.1 state that antibiotic therapy is recommended for patients with signs of local or systemic inflammatory response and/or adjacent or contiguous collections. On the other hand, indications for surgical treatment are inadequate response to conservative management, uncertain diagnosis despite complementary tests, onset of complications (pulmonary thromboembolism), extension of thrombus into the external inguinal ring, and patients at high risk for new episodes of venous thromboembolism 1,20.
Although rare, SVT complications include testicular infarction, complicated inguinal hernias 12, extension of the thrombus into the renal vein, and even secondary pulmonary thromboembolism 21. The course of this condition is often benign and usually controlled with medical treatment, even though its diagnosis is often post-surgical.
The present case is relevant because it is the third of its kind reported on the right side worldwide 1,9 and because a favorable outcome and an acceptable follow-up were achieved. The limitations of this report include the fact that no specific etiology was found to explain the onset of the disease.
CONCLUSIONS
SVT is rarely observed, and its etiology may be associated with multiple factors, which makes it a diagnostic challenge. This condition is one of the differential diagnosis of acute scrotum pain and is, therefore, usually observed after surgical examination. Doppler ultrasound is the preferred method to confirm its presence due to its low cost; nevertheless, angiotomography may be required when thrombus extension is suspected.
SVT treatment is conservative in most cases and includes anticoagulant therapy, anti-inflammatory drugs, antibiotics (in case of inflammatory process), local therapy, and clinical follow-up. In the event of complications, diagnostic doubt and poor response to conservative treatment, surgical management with thrombus excision and/or vein ligation may be considered.
Knowledge of this disease allows medical personnel to suspect it and provide the patient with timely treatment to obtain good outcomes; in this sense, the publication of this case is relevant to know a little more about such a rare entity.
PATIENT PERSPECTIVE
At the time of the last check-up, the patient said he was pleased with the outcomes of his treatment and that he was willing to follow all the recommendations given to him. He also expressed his gratitude for the opportunity to contribute with his case to the scientific literature and thus broaden the knowledge about this disease.














