INTRODUCTION
Clear cell chondrosarcoma is a rare subtype of benign tumor (2% of all chondrosarcoma cases) 1 that predominantly affects young adults and involves the epiphyses of long bones, especially the femur and proximal humerus 2-4. This type of neoplasm can be mistaken for other cystic lesions due to its imaging characteristics; moreover, there are no clear guidelines for its treatment and outcomes to date.
The following is the case of a patient with clear cell chondrosarcoma in the proximal tibia at the level of the medial tibial plateau who was successfully treated with en bloc excision with tumor-free margins, structural allograft, and stabilization with tibia proximal plate.
CASE PRESENTATION
A 46-year-old Caucasian woman from Bogotá (Colombia), a civil engineer with no significant medical or surgical history, consulted the oncology orthopedic department of a quaternary care institution in November 201 9 due to chronic pain in the medial left knee at the level of the proximal tibia for 8 months that woke her up at night and forced her to use a cane as an external support while walking. The patient reported having attended physical therapy sessions and using oral analgesia without improvement.
On physical examination, the only finding was tenderness to palpation at the medial tibial plateau of the left knee associated with edema; the range of motion at the joint was normal and there were no clinical signs that suggested ligamentous or meniscal lesions. Considering these findings, diagnostic imaging studies (X-ray and MRI) were performed.
Conventional knee radiographs (Figure 1) showed a small round epiphyseal lytic lesion with well-limited borders at the medial tibial plateau, although no periosteal reaction or other associated changes suggesting local aggressiveness were observed.

Source: Document obtained during the study.
Figure 1 Anteroposterior and lateral knee radiographs showing a lytic lesion at the medial level of the proximal epiphysis of the left tibia.
On the other hand, magnetic resonance imaging (MRI) (Figure 2) showed a prominent and confluent bone and subchondral cysts of 18mm in diameter in the medial tibial plateau, as well as a diffuse increase in bone marrow signal intensity and changes associated with disuse osteopenia.
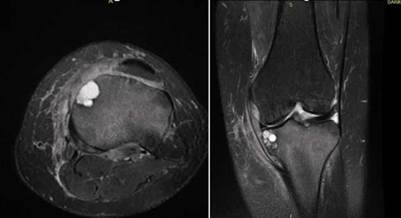
Source: Document obtained during the study.
Figure 2 MRI of the left knee in T2 mapping sequence in axial and coronal view showing a cystic lesion in the medial tibial plateau and a diffuse increase in the signal intensity of the tibia.
Taking into account the clinical and imaging findings, an epiphyseal chondroblastoma or giant cell tumor were initially suspected as the main differential diagnosis. Consequently, an open biopsy was performed, which macroscopically showed a chondral lesion with sclerotic edges and no involvement of the articular cartilage of the tibia. Microscopically, it showed nests of epithelial clear cells that led to suspect between metastases or clear cell chondrosarcoma.
Immunohistochemistry of the lesion proved positive for vimentin, S100 and D2-40 proteins and negative for antibodies AE1/AE3, CK7, CK20, PAX8, PAX2, NAPSIN-A, RCC, which supported the diagnosis of clear cell chondrosarcoma. Further tests were performed, including thoracic and abdominopelvic tomography, which were negative for distant metastasis.
Based on these findings and the rare occurrence of clear cell chondrosarcoma, the following month the case was brought to a multidisciplinary board (orthopedic oncology, musculoskeletal radiology, oncology, surgical oncology, radiotherapy, and pathology services), in which, by consensus, complete surgical resection of the lesion was decided upon.
The surgery was performed on January 7, 2020, using an anteromedial approach to the proximal tibia. During this procedure, the biopsy trajectory and the described lesion were removed, with tumor-margins of approximately 2cm. The medial tibial plateau was resected, and the ligamentous and meniscal structures of the knee were preserved (Figure 3). The bone defect was also managed by applying a structural corticocancellous allograft (Figure 4) that was stabilized with a proximal tibia plate, thus achieving recovery of the joint surface and the anatomy of the proximal tibia (Figure 5). There were no complications during the procedure.

Source: Document obtained during the study.
Figure 3 Picture taken during the procedure showing oncologic resection of the chondral lesion at the level of the medial tibial plateau.

Source: Document obtained during the study.
Figure 4 Allograft of corticocancellous bone at the level of the proximal tibia.

Source: Document obtained during the study.
Figure 5 Postoperative x-ray showing recovery of the joint surface and proximal tibia anatomy.
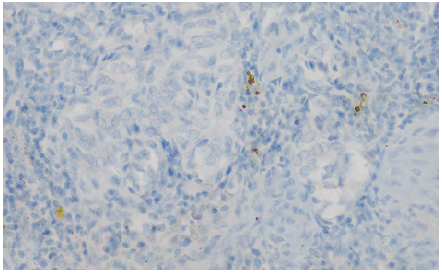
Histopathological analysis revealed a lesion composed of nests of clear cell (Figure 6) surrounded by mixed inflammatory infiltrate without clear chondroid differentiation, findings that raised suspicion of metastatic carcinoma, melanoma, and clear cell chondrosarcoma. Clinically, there were no lesions at other sites where metastasis was suspected. An immunohistochemistry study was performed, finding reactivity for S100 (Figures 7 and 8) with negativity for cytokeratins (AE1AE3), anti-endomysial antibodies (EMA), and me-lanocytic markers HMB45, Melan A, and SOX10. These findings were consistent with clear cell chondrosarcoma with negative tumor margins.
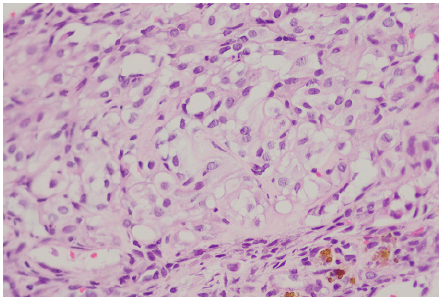
Source: Document obtained during the study.
Figure 6 Histopathological analysis showing nests of clear cells.
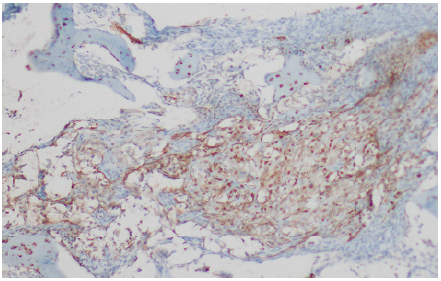
Source: Document obtained during the study.
Figure 7 Histopathological analysis showing positivity for S100 in tumor nests and negativity for melanocytic markers.
Source: Document obtained during the study.
Figure 8: Histopathological analysis showing negative cytokeratin cocktail in tumor cells.
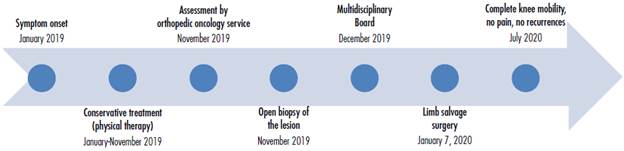
After the procedure, the patient began a rehabilitation process with initial non-weight bearing. Five months after the procedure, she no longerfelt pain and was able to achieve full mobility of the knee and walk without limping and using only one crutch. Likewise, her clinical condition continued to be followed up using diagnostic imaging. At the time of writing this report, she had not presented any tumor recurrence and had an adequate integration of the allograft observed during radiographic follow-up. Figure 9 presents the case timeline.
DISCUSSION
Chondrosarcoma is the third most common type of bone tumor after myeloma and osteosarcoma, with conventional central chondrosarcoma being the most frequent (85% of all cases) 5. Clear cell chondrosarcoma, which was first described by Unni etal. in 19766, is a rare variant of low-grade chondrosarcoma (2-4% of all cases) 2,7 mostly observed in men aged 20 to 40 years. Together with mesenchymal chondrosarcoma and dedifferentiated chondrosarcoma, it is one of the rare subtypes due to its histological and clinical characteristics 1.
Conventional chondrosarcomas originate mainly in the pelvis, shoulders, and ribs, while clear cell chondrosarcomas usually occur in the epiphyses of long bones, being more common in the femur and proximal humerus 2-4. Even though there are reports of dedifferentiated clear cell tumors, they are usually low grade, so cases of metastasis are rare and, if they occur, mainly affect the lung and brain 4.
Since it is a slow-growing, low-grade lesion, clear cell chondrosarcoma can be mistaken for bone cysts on diagnostic imaging and therefore diagnosed late. In conventional x-rays, they are seen as expansive radiolucent lesions of cystic or lobulated appearance with reactive cortical thickening, without destruction of the cortical layer nor periosteal or soft tissue involvement. 3,4 In computed tomography, they can be identified as calcifications of the chondroid matrix with sclerotic contour and cortical involvement 3.
Given these findings, differential imaging diagnoses are usually simple or aneurysmal bone cysts, giant cell tumor, chondroblastoma, enchondroma, and chondromyxoid fibroma. No imaging findings are specific to this type of tumor, so biopsy with histopathological and immunohistochemistry analysis is decisive to confirming the diagnosis 4.
On histopathological analysis, clear cell chondrosarcomas appear macroscopically as gray or whitish masses with areas of mineralization, and not as hyaline areas typical of chondrosarcomas 8. On the other hand, on microscopic analysis, characteristic clear cells are observed in lobules or sheets infiltrating the trabecular bone and have centralized, round or oval nuclei with clear cytoplasm and well-defined borders. In addition, some areas of the tumor usually show characteristics of a conventional chondrosarcoma with hyaline areas 4,8,9. It is worth noting that although these are low-grade tumors, an increase in metalloproteinases 2 (MMP-2) may be associated with the behavior of a tumor with a high risk of metastasis 10,11.
Both clear cell chondrosarcoma and chondroblastoma show epithelioid and chondrogenic cell characteristics. Immunohistochemistry is a useful tool for confirming the diagnosis of the former since this procedure is positive for type II collagen, vimentin and S100, and negative for EMA and cytokeratin 9,12,13. In this regard, it should be noted that the most important differential diagnoses in epiphyseal lesions are chondroblastomas, which are usually more frequent in adolescents and present individual calcifications and pink cartilage nests on diagnostic imaging and are positive for DOG-1 in immunohistochemistry. Other differential diagnoses are giant cell tumor, carcinoma, and melanoma. In immunohistochemistry, carcinoma is positive for epithelial markers such as cytokeratins and epithelial membrane antigen, while melanoma is reactive for melanocytic markers such as Melan A, HMB-45, and SOX10 14-16.
The mainstay of treatment for clear cell chondrosarcoma is surgery, in which a wide excision with free of tumor at the margins of at least 5mm 2,4,8 should be performed. Long-term follow-up is essential in the management of these tumors because, as Kang et al.9 stated in their case report, simple excision or intralesional curettage can cause recurrence and metastasis in more than 80% of cases. However, Klein et al.12 state that these values are lower (30% and 15%, respectively) in follow-ups at less than 10 years. The latter authors also found a correlation between shorter survival and previously identified risk factors for chondrosarcoma: positive margins and metastases. 12
Chemotherapy and radiation therapy are ineffective to treat clear cell chondrosarcomas; however, they may be indicated as adjuvant or palliative treatments when metastases occur and in inoperable cases 4.
There is no clear evidence in the literature regarding the prognosis of clear cell chondrosarcomas due to the low incidence of these tumors. However, Itälä et al.17 reported that, in their study, the overall 10-year survival of patients with these tumors was 89% and disease-free survival was 68%.
The case presented here is noteworthy because clear cell chondrosarcoma was found in an unusual location (tibial plateau) that is little described in the literature, and because the diagnosis was delayed due to subtle changes in radiographic images, with immunohistochemistry being the primary tool for confirmation. Surgical therapy was chosen for this patient, including free-margin resection and allograft reconstruction of the proximal tibia. Even though the results obtained with this management were satisfactory, and there was no evidence of tumor recurrence at the time of writing this report (medium term), prognosis may change in the long term and the patient may present with arthroscopic changes of the knee and require new interventions.
CONCLUSIONS
This is the case of a patient with a very rare subtype of chondrosarcoma found in an unusual location, who presented chronic knee pain and subtle changes on imaging studies. Given the nonspecific nature of the symptoms, the diagnosis of clear cell chondrosarcoma was made 8 months after their onset, and immunohistochemistry was the key tool to rule out more frequent differential diagnoses. Resection with free margins of neoplastic infiltration and reconstruction with proximal tibial allograft were performed, with which the functionality of the knee was restored, and the pain disappeared.