INTRODUCTION
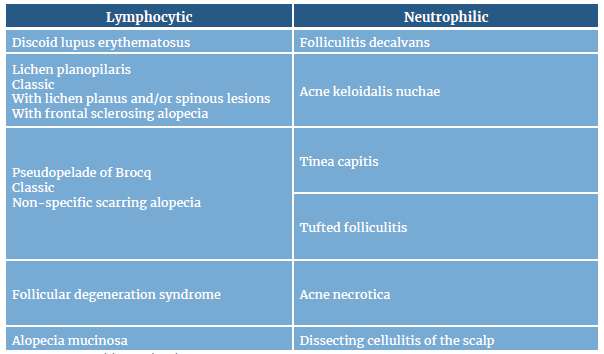
Folliculitis decalvans, also known as scarring alopecia, is a type of primary cicatricial alopecia (for a description of the different types of primary cicatricial alopecia see Table 1) 1. It is a rare skin disease characterized by the presence of inflammatory neutrophilic infiltrates and scarring that cause perifollicular papules and pustules, and it accounts for approximately 10 % of all primary cicatrizing alopecia cases 2,3. This condition was first described by Quinquaudin 1888 3,4, but it was only until 1905 that it was named as folliculitis decalvans by Broqc et al. 5
It generally occurs in middle-aged adults, predominately males, and tends to be more frequent in people with dark skin. Although its etiology is unknown, it has been described that Staphylococcus aureus may be a contributing factor; 6-8) other possible causes include mechanisms involving superantigens or cytotoxins that bind to themajor histocompatibility complex class II (MHC II) molecules 9 and a genetic component, since several familial cases have been reported. 2,10,11
Folliculitis decalvans management has proven to be a challenge since there is a wide range of treatment alternatives, including antibiotic therapy (tetracycline, trimethoprim/sulfamethoxazole, cephalosporins, ciprofloxacin, minocycline or clindamycin or clarithromycin plus rifampicin) 1,6,9, the use of topical antibiotics (for example erythromycin, mupirocin and clindamycin) 1, antifungals, retinoids, corticosteroids (topical or oral), phototherapy, and laser depilation. 1,7,12
The occipital region and the vertex are usually the most affected areas in patients with this condition. Generally, folliculitis decalvans starts as a single lesion and then spreads in a centrifugal progression with the development of painful follicular papules and pustules. 2,5 As the disease progresses, a hardened erythematous plaque appears. 7 Follicular keratosis, erosions and hemorrhagic crusts are also observed. 5,13 Furthermore, some patients may experience spontaneous bleeding, pain, and a burning sensation. 5,6 Likewise, polytrichia (tufted hairs), that is, the presence of multiple hair shafts emerging from a single dilated hair follicle, may also be found in some cases. 5,6,9,14
Dermatoscopy has been shown to be a useful procedure for diagnosing this skin condition. 15 In this regard, trichoscopy can be highly useful. In patients with folliculitis decalvans, the main finding during this examination is the presence of tufted hairs surrounded by perifollicular hyperplasia that may be arranged in a starburst pattern (starburst sign); other findings include the presence of yellowish tubular scaling and follicular pustules with emerging hair shafts in their midpoint. In addition, white and milky red areas lacking follicular openings are predominant in long-lasting lesions. 16,17
Histopathologically, these lesions are first characterized y by the presence of neutrophilic infiltrates, and, as it progresses, the presence of neutrophilic, lymphocytic and histiocytic infiltrates. 18 At first, the location of the infiltrate is peri-infundibular, but it may affect the entire follicle. 18,19
Other usual findings in patients with folliculitis decalvanas include the formation of abscesses and the presence of polythrichia and perifollicular fibrosis. 19 Infectious agents are rarely found and differential diagnoses include infectious folliculitis, follicular degeneration syndrome, and acne necrotica. 1 This paper reports the case of a young healthcare worker with folliculitis decalvans.
CASE PRESENTATION
This is the case of a 26-year-old middle-class male healthcare worker of Hispanic origin, from Bogotá D.C., Colombia, who, in August 2017, visited the outpatient service of a tertiary care hospital due to a history of approximately 4 years of pustules and papules in the scalp.
According to the patient, he did not have any relevant history of disease or surgeries. He reported drinking alcohol occasionally but denied having used psychoactive substances; also, he did not have any known allergy. The patient had the following family history of disease: gastric cancer (paternal grandmother), breast cancer (half-sister), and diabetes mellitus type 2, hypertriglyceridemia, and high blood pressure in other relatives, both maternal and paternal.
The following findings were reported on the physical examination made during the outpatient appointment: blood pressure: 118/76; heart rate: 64 bpm; respiratory rate: 16 bpm; body temperature: 36.6°C; weight: 91kg, and height: 168cm. Likewise, several lesions (approximately 60) compatible with perifollicular papules and pustules were observed mainly on the scalp (in the vertex and the occipital, temporal, and parietal regions), while some others were located in the bordering area between the neck and the scalp.; there were no lesions in other regions different than the scalp, that is, the face, armpits, groin or buttocks. Regarding its mental health status, the patient reported feeling irritable and having a negative attitude due to the lack of sleep experienced as a result of the pain produced by the lesions. There were no other significant findings.
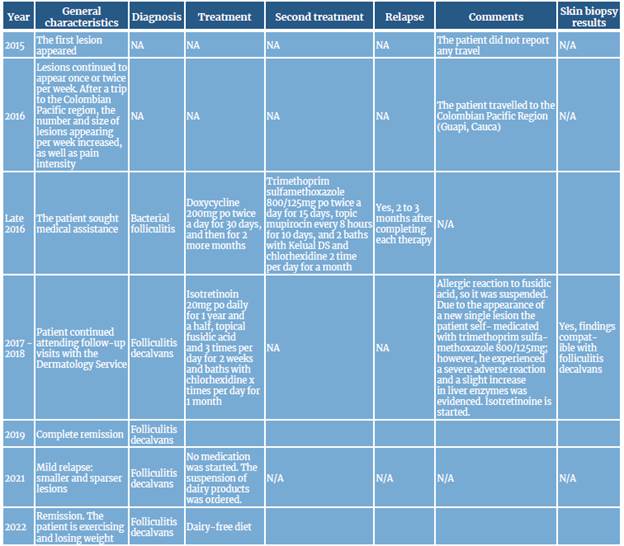
During the 2017 outpatient appointment, the patient reported the following sequence of events.
August 2015: The patient reported that he started suffering from individual and extremely painful and suppurating pustules since the second semester of 2015. In addition, according to the patient, each lesion had the same rapid evolution, described as follows: 1) development of painful erythema, 2) increase in the severity of erythema and swelling, 3) appearance of a pustule, and 4) spontaneous pustule rupture with blood and purulent fluid (pus) secretion. (Figure 1A). Most of the lesions appeared in the occipital region of the scalp. This situation persisted over time, but as there were very few lesions, he did not did not seek medical help. According to the patient, the appearance of the first lesions was caused by a prolonged and seriously stressful situation.
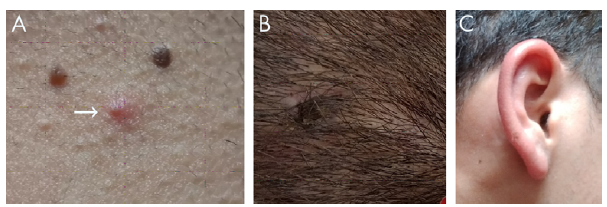
Source: Images obtained while conducting the study.
Figure 1 A) A pustule on the scalp, more specifically in the bordering area between the scalp and the neck. B) Site of the skin biopsy, near the vertex. C) Erythematous swelling secondary to the application of fusidic acid.
October 2016: After a trip to the Colombian Pacific region, the patient started to notice an increase in the number, distribution, and size of lesions. At first, he reported that 1 or 2 lesions would appear per week, but that as time passed this number increased to 30 or more per week. Also, not only the number of lesions appearing per week increased, but they started to appear in other regions of the scalp different than the occipital region, including the vertex an the temporal, and parietal regions. As a result of such an increase in the number of lesions and their wider distribution, e pain became almost unbearable, thus affecting his sleep habits and mood.
Late 2016: Given this situation, the patient scheduled a medical visit with a general physician who diagnosed him with bacterial folliculitis and started treatment consisting of doxycycline 200mg per os twice per day for 30 days, although he did not have a history of head shaving. In addition, the patient was referred to a dermatologist for further assessment, who agreed with continuing the initial antibiotic therapy for two more months, achieving the complete resolution of the existing lesions.
February 2017: Unfortunately, about two to three months after ending the doxycycline therapy, the lesions reappeared, so the patient scheduled another medical appointment with the same dermatologist and a new antibiotic treatment was started, this time consisting of oral trimethoprim/sulfamethoxazole 800mg/125mg twice a day for 15 days, topical mupirocin every 8 hours for 10 days and taking showers/baths with Kelual DS foaming gel (ciclopiroxolamine) and ch-lorhexidine 2 times per day for a month. As was the case with the initial suggested treatment, lesions disappeared, but they reappeared two to four months later.
June 2017: The patient reported that pain intensity and the number and size of lesions increased each time there was a relapse. Also, he said that some lesions were fusing together (3 to 5 at a time), and that he had observed alopecia in some areas. Likewise, he expressed having problems to sleep due to the pain caused by the lesions, as well as subsequent irritability and mood swings, which had a negative impact on his life both personally and the at the workplace. He also reported that his sister had started to experience similar signs and symptoms although less severely.
November 2017: Despite the reappearance of the lesions, no pharmacological treatment was prescribed by the dermatologist until a skin biopsy was performed, since folliculitis decalvans was suspected. The skin biopsy was performed using samples taken from two lesions (Figure 1B). Diagnosis was confirmed with biopsy report results (January 2018), in which the following findings were described: neutrophilic infiltrates, perifollicular fibrosis and polytrichia (no cultures were taken). Once the diagnosis was confirmed and routine laboratory tests were performed, that is, late January 2018, the patient was prescribed with oral isotretinoin therapy (20mg daily) for a year and a half due to his weight, as well as the use of topical fusidic acid 3 times per day for 2 weeks and taking baths with chlorhexidine 1 time per day for 1 month; he was also informed of some recommendations, such as stopping alcohol consumption altogether.
After treatment was started, the patient's condition improved significantly as lesions and alopecia areas disappeared. However, he reported having an allergic reaction to fusidic acid, so its use was immediately suspended (Figure 1C). Approximately 4 months after the treatment was started, a new lesion appeared, but he opted for self-medication (a single dose of trimethoprim/sulfamethoxazole of 160/800mg), which caused a severe adverse reaction (fever, headache, and fatigue), so he suspended the use of this antibiotic; there were no more self-medication cases during the remaining of the treatment after it was finally completed. The results of the laboratory tests taken at different times (diagnosis and treatment over one year and a half), including those performed after the adverse reaction to trimethoprim/sulfamethoxazole occurred, are available in Table 2.
Table 2 Laboratory tests results of the patient.
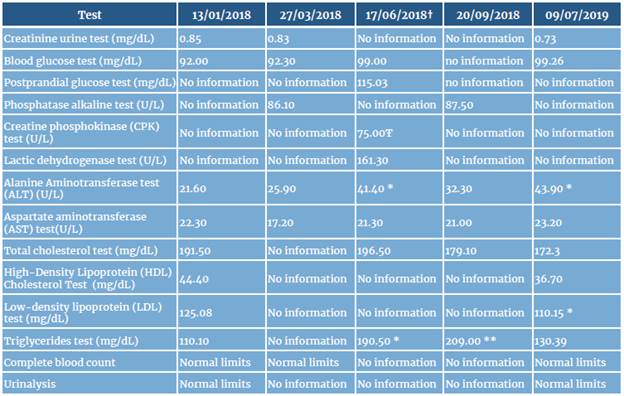
Comments:
* Outside normal reference values; slight increase in values.
** Outside normal reference values, significant increase in values.
† Prior to undergoing these tests, the patient self-medicated.
Ŧ There was no control CPK test, which is another limitation of the case presented here.
Source: own elaboration based on the data obtained from the patient's medical record.
November 2019: Treatment was completed without any adverse effects. It should be noted that despite medical treatment was started relatively early and complete remission was achieved, there is always a possibility of relapse. A yearly timeline of the case is described in Table 3.
November 2021 (follow-up): The patient reported a mild relapse. However, lesions disappeared after he followed the recommendation of suspending the consumption of milk and other dairy products.
January 2022 (follow-up): According to the patient, lesions do not appear unless he consumes dairy products or derivatives, as they usually appear 2 to 3 days after he eats or drinks any of such products, but they disappear within 2 to 3 weeks after suspending said consumption. There was no sign of new lesions during this follow-up examination, and the patient claimed that he is doing his best to continue with a dairy-free diet.
DISCUSSION
Folliculitis decalvans is a rare type of primary cicatricial alopecia that mainly affects middle-aged males 18,19,20,21. In addition, although it has been described that S aureus infection might be a contributing factor, there is no clear evidence on its association with the occurrence of this disease 18,19,20,21. Most cases seem to be sporadic, and lesions mainly appear on the vertex. 20,21 Its diagnosis and treatment are a challenge since reaching a diagnosis may take several years and sometimes treatment needs to be extended due to folliculitis decalvans being refractory. 22
In the case reported here, the information provided by the patient allowed the treating physician to make a rather fast diagnosis and start a timely treatment. The clinical manifestations of folliculitis decalvans described here are similar to what have been reported in other case reports 6,9. Likewise, as shown in other case reports 23, treatment with isotretinoin was successful in our case. Other therapeutic options include the use of biological drugs, 24,25 photodynamic therapy 20,21 and even YAG laser 26, especially in cases of recalcitrant folliculits decalvans.
Regarding prognostic factors for severe folliculitis decalvans, our patient presented with tufted hairs (polytrichia); besides it had an early onset (age < 25 years old) and had lasted several years. 20) As mentioned above, proper treatment of this condition has proven to be a challenge 1,7,12, as several therapies have been reported with a varying range of success; in this regard the main clinical characteristics of folliculitis decalvans, as well as some of the therapies described for its treatment (including doses) are available in Table 4. Other therapeutic alternatives include medical honey 27 and adipose tissue transplantation. 22) Primary scarring alopecia refers to a heterogeneous group of rare disorders in which hair follicles are destroyed irreversibly, 28 most of these disorders can be easily recognizable based on their clinical manifestations, however skin biopsies are useful for confirming the diagnosis. 29
Table 4 Treatment options and main clinical characteristics of folliculitis decalvans and some other types of scarring alopecia.
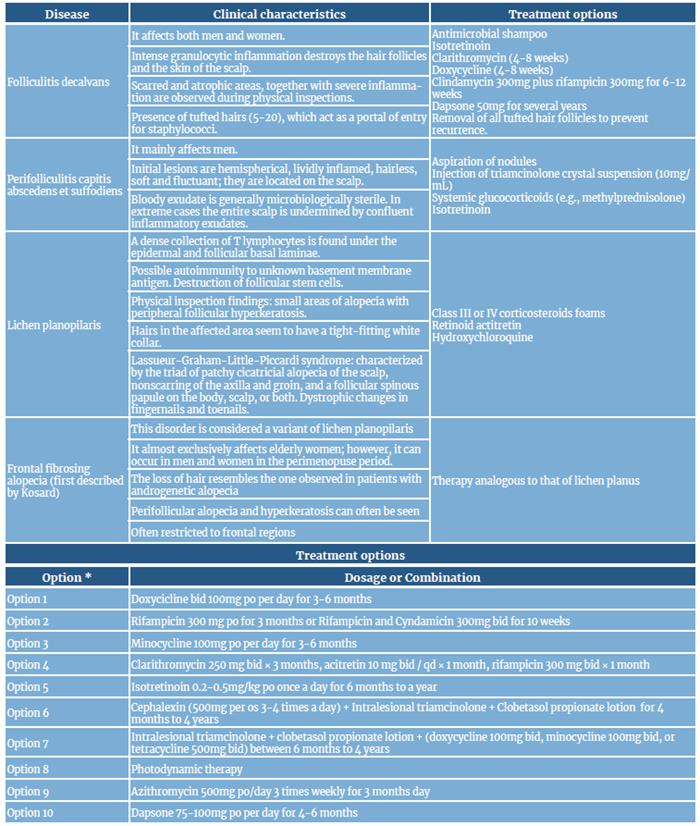
bid: twice a day
po: medication taken orally
qd: every day
* There are many other therapeutic options available. Treatment of the disease is not clear, as it can last even years and there is not strong evidence supporting its implementation. 40
Source: Own elaboration based on Powell et al.6; Sillani et al.9; Miguel-Gómez et al.20; Tietze et al.23; Trüeb 28; Wolff et al.30; Stokmeier et al.31; Bolz et al.32; Kossard 33; Vaño-Galván et al.34; Harries & Messenger 35; Le Cleach & Chosidow 36; Tan et al.37; Miguel-Gomez et al. 21; Vaño-Galván et al. 2; Bunagan et al.38; Aksoy et al.39, and Rambhia et al.40.
Although the use of isotretinoin is a valid therapeutic alternative for the treatment of folliculitis decalvans, it can cause several adverse effects on the skin and mucous membranes, as well as muscle and skeletal alterations; besides, its teratogenic effect may limit its usefulness. 22
The management of folliculitis decalvans requires both patience and economic resources, for its treatment is lengthy, and the medications to be used may be expensive. In this regard, it has been estimated that a patient might spend as much as 80 sterling pounds per month ($99 USD) in medications and other products necessary for proper treatment. 20
On the other hand, patients with this condition need to be aware of the importance of follow-up and their own responsibility in terms of adherence to treatment and the proper care of the lesions; for example, in the case of our patient, he was asked to completely stop drinking alcohol due to the metabolism of isotretinoin. Furthermore, patients must be informed that the possibility of relapse is always present, and that it may take years to achieve full remission (i.e., absence of folliculitis decalvans), or that even treatment will be needed the whole life; making this clear early is important because it may have a toll on the patient's mental health. 20 Likewise, patients must be aware of the challenges of reaching a diagnosis, as folliculitis decalvans is not only a rare disorder, but there are also several differential diagnoses (Table 5).
Table 5 Differential diagnoses of scalp folliculitis.
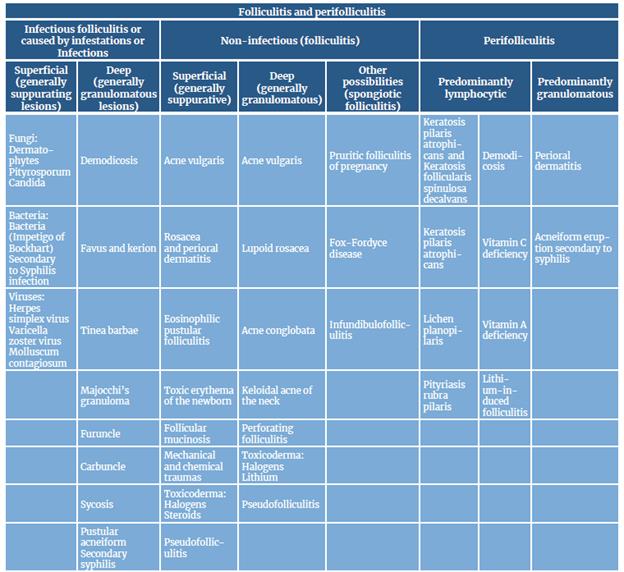
Source: Own elaboration based on the paper by Lugovic-Mihic etal.41, which in turn used information described by Camacho et al.25
One of the most important strengths of the case reported here is that the patient was referred to the dermatology service for conducting a comprehensive assessment consisting of a thorough clinical and physical examination and the performance of laboratory tests and a skin biopsy. On the other hand, this case has the following limitations: genetic and immunological aspects were not analyzed; the patient's relatives were not assessed and tested and, therefore, it was not possible to confirm the presence of familiar cluster; there were no follow-up laboratory tests; and there were no photographs depicting the histopathological characteristics and clinical distribution of the lesions.
CONCLUSION
The case reported here clearly exposes the challenges that treating folliculitis decalvans and other types of primary cicatricial alopecia implies. In addition, this case is of great importance since, if further genetic testing is performed, the possible presence of a familial cluster of folliculitis decalvans could be confirmed.
Furthermore, it was observed that although the patient had an adequate response to retinoid therapy, drug interactions must always be monitored to avoid the occurrence of adverse reactions, as happened when the patient self-medicated with trimethoprim sulfamethoxazole while taking isotretinoin, even though no adverse reactions were reported when such treatment was first implemented.