INTRODUCTION
De Garengeot hernia is a femoral hernia that contains the appendix. It was first described in 1731 by René Jacques Croissant de Garengeot and, according to the literature, the first case of appendicectomy due to appendicitis contained in a De Garengeot hernia was published in 1785 by Hevin 1,2. This type of hernia is most common in women, accounts for only 0.5% to 5% of all hernias, and can lead to complications such as strangulation or acute inflammation in some cases 1.
Differential diagnoses of De Garengeot hernia include Amyand hernia, which is defined as an inguinal hernia that contains the appendix; pelvic or venereal infectious diseases associated with adenopathies; incarcerated or strangulated hernias; soft tissue tumors, among others 3-5. Although its diagnosis is usually clinical, diagnostic imaging must be used to establish pre-surgical planning. It is important to keep in mind that in most cases this type of hernia is diagnosed intraoperatively 1-3.
The main approaches proposed for the management of this entity are appendectomy and herniorrhaphy 4,6.
The following is the case of a woman with a De Garengeot hernia and multiple comorbidities, who was diagnosed via ultrasound and had inflammation of the tip of the appendix during her treatment.
CASE PRESENTATION
A 75-year-old white woman attended a primary health care center due to pain and mass sensation in the right inguinal region for a month. The patient reported the following relevant history: chronic hypertension, active smoking, and pulmonary thromboembolism, which was treated with low molecular weight heparin.
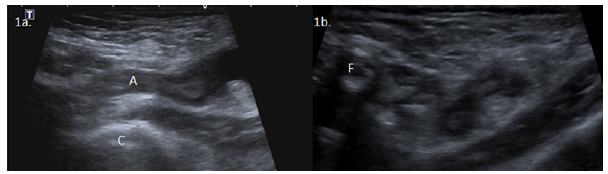
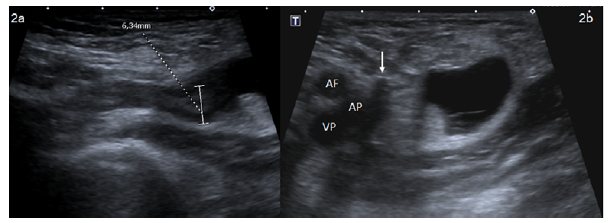
An ultrasound of the inguinal region performed shortly after the onset of symptoms revealed a De Garengeot hernia of 6.3mm in diameter that did not compress with external pressure during the examination. This imaging study also revealed fluid with thin septa inside the hernia sac (Figures 1 and 2), so the patient was advised to go to the emergency department. However, the woman opted to wait and consult on an outpatient basis, and one month later attended the general surgery service of the Hospital Universitario Nacional de Colombia.
Source: Document obtained during the study.
Figure 1 Ultrasound of the inguinal region along the longitudinal axis (1a) and the transverse axis (1b). A: vermiform appendix; C: femoral head; F: common femoral artery.
Source: Document obtained during the study.
Figure 2 Ultrasound of the inguinal region. 2a) thickening of the tip of the appendix; 2b) fluid with thin septa inside the hernia sac. Arrow: compression of the medial wall of the femoral vein: AF, superficial femoral artery; AP: deep femoral artery; VP, deep femoral vein.
On admission examination, vital variables were altered: heart rate of 66 bpm, respiratory rate of 14 rpm, blood pressure of 107/48 mmHg, and oxygen saturation of 88% with FiO2 of 0.28%. On physical examination, the patient was found in acceptable general condition, conscious and hydrated; her abdomen was soft, and, on palpation, there was no evidence of pain, masses, signs of intestinal obstruction, increase in the size of the abdominal organs, or distension. A mass of 3cm in diameter was found in the right inguinal region; it was painful on palpation and did not compress with external pressure. The rest of the examination was normal.
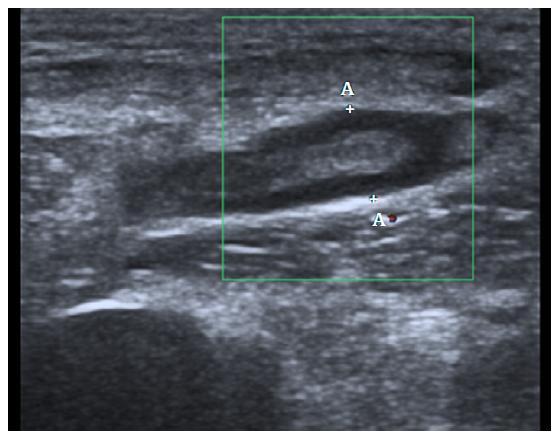
Based on the findings of the physical examination and the initial ultrasound, it was decided to hospitalize the patient and perform a series of pre-surgical laboratory tests, all of which were within normal ranges. An ultrasound study was performed again, confirming the presence of a De Garengeot hernia and showing that the vermiform appendix had a thickening in the walls of its tip, with an anteroposterior diameter of 6.7mm that did not decrease with external pressure, as well as scarce free fluid in the hernia sac (Figure 3).
Source: Document obtained during the study.
Figure 3 Follow-up ultrasound performed one month after the onset of symptoms showing cecal appendix with thickening of the appendix wall and contained within the hernia sac.
Following an assessment by the Internal Medicine Service, done considering the patient's comorbidities, and after completing the recommended of anticoagulant suspension, the woman was taken to surgery 24 hours after admission. Under general anesthesia, an appendectomy was performed using a preperitoneal approach with access to the abdominal cavity; a polypropylene preperitoneal mesh was placed to correct the femoral hernia.
The patient recovered well from the surgery and was discharged the following day. During a postoperative follow-up visit performed after 44 days, the woman was asymptomatic, with the surgical wound in good condition, and no hernia reproduction nor signs of infection.
DISCUSSION
De Garengeot hernia occurs most often in women; some of the conditions that may favor its appearance are pregnancy, smoking, constipation, advanced age, and connective tissue disorders 1,2,4. This entity accounts for about 1% of all femoral hernias and can cause acute appendicitis in up to 0.13% of cases.
One theory proposed to explain the development of De Garengeot hernias refers to the abnormal attachment of the appendix to the cecum, while another suggests that the presence of a large cecum may push the cecal appendix into an existing femoral defect.
The clinical spectrum and physical examination findings in cases of De Garengeot hernia may include abdominal pain, fever, local inflammation, and inguinal masses that do not diminish in size with external pressure or supine position. Differential diagnoses include Amyand's hernia, adenitis, annexitis, and soft tissue tumors 2-4,7.
Most femoral hernias are diagnosed clinically and further evaluated with diagnostic imaging; however, De Garengeot hernias are usually diagnosed during surgery. In this sense, in the presence of an inguinal mass with clinical suspicion of hernia, a confirmatory ultrasound should be performed, as this is the method of choice for such entities due to its wide availability, low cost, and high efficacy. In this regard, Robinsón et al. 8, in a study of 59 patients performed to investigate the accuracy of ultrasound in patients with symptoms suggestive of hernia, found that although this is an operator-dependent test, it can help characterize the type of hernia with a sensitivity of 90%, a specificity of 91%, a positive predictive value of 68%, and a negative predictive value of 98% if the person performing the test has adequate training.
Ultrasound is also a useful tool in the follow-up of patients with previous surgeries. For an adequate exploration, it is necessary to use equipment with high frequency linear transducers, preferably >10 MHz, which allows us to obtain imaging with high spatial resolution and anatomical detail to identify the structures that delimit the inguinal region, particularly the Hesselbach's triangle: the inferior epigastric vessels, the inguinal ligament, and the lateral border of the rectus abdominis. Moreover, other structures such as the spermatic cord, femoral vessels and the conjoint tendon, formed from the lower part of the common aponeurosis of the abdominal internal oblique muscle and the transversus abdominis muscle, can be assessed using this imaging study. Exploration should be performed carefully to obtain images in orthogonal planes at rest and with the Valsalva maneuver in order to not only locate the structures of the Hasselbach's triangle, but also to determine the size of the defect or neck of the hernia and the hernia sac, as well as the characteristics of its contents 9.
Femoral vein compression is a particular finding described for femoral hernias on ultrasound and tomography; this happens because hernias pass through the lower part of the inguinal ligament, where the hernia sac and its contents exert pressure on this vein. It should be noted that computed axial tomography is useful not only for diagnosing femoral hernias, but also for ruling out other diagnoses 10.
Femoral hernias are associated with an increased risk of incarceration of the herniated contents, which may result in acute appendiceal inflammation, and this is believed to be related to external compression of this organ at the neck of the hernia. Perforation and peritonitis are less frequent complications because pelvic rigidity prevents the spread of inflammation to the peritoneal cavity 4,11; necrotizing fasciitis may also occur on some occasions.
Patients with De Garengeot hernia should be taken to surgery as soon as they are diagnosed and necessary pre-surgical examinations are available. Currently, there are no unified standards about the type of intervention to be performed; therefore, it is recommended that surgeons decide the most appropriate surgical strategy based on their experience and case characteristics. Some of the options for performing the surgery include localized open approaches, midline laparotomy, and laparoscopic-assisted approaches 11,12.
The use of prosthetic materials to repair the hernial defect is controversial when the cecal appendix is inflamed due to the risk of mesh contamination, which can lead to a variety of complications, the most common of which is operative site infection (30% of cases) 4,5,7.
In the case presented here, ultrasound was used to make the diagnosis, as well as to determine the cause of the patient's symptoms and to devise a suitable surgical plan; the surgical intervention included appendectomy and hernia repair with prosthetic material. Similarly, the histopathological report indicated a cecal appendix with follicular lymphoid hyperplasia, that is, the inflammation of the appendix observed on ultrasound was limited. This case was successfully treated and had a favorable outcome, allowing the patient to improve her quality of life as a result of symptom resolution.
CONCLUSION
De Garengeot hernia is a rare condition that is usually diagnosed intraoperatively; however, diagnostic imaging is the primary tool for characterizing these hernias when performing a mass assessment of the inguinal region. In the case presented, the diagnosis was made using ultrasound, which has a high degree of sensitivity and specificity, and is low cost and easy to perform.
To avoid complications, surgical management of a De Garengeot hernia should be established as soon as possible. In this case, appendectomy and mesh hernia repair were the primary treatments, but it should be noted that the patient did not have appendicitis or infection.














