INTRODUCTION
Inflammatory diseases of the bone system include clinical entities characterized by unifocal or multifocal lesions in the bone without evidence of associated infectious involvement 1,2.
Regarding the pathophysiology of such diseases, it has been proposed that dysregulation of the innate immune system is a crucial factor in their genesis and development. Experimental evidence has demonstrated that alterations in the functioning of inflammatory cells can affect any body tissue, including bone tissue, where an abnormally persistent cycle of resorption and remodeling may occur in response to certain chemical mediators secreted by inflammatory cells 2-4. Additionally, specific mutations affecting molecules related to different inflammatory pathways have been described in humans and animal models 3.
Chronic recurrent multifocal osteomyelitis (CMRO) is a rare inflammatory bone disease that mainly affects children and adolescents and can be mild and self-limited or chronic and recurrent, with varying degrees of severity 1,2. Management guidelines to control symptoms, as well as to prevent or slow the progression of bone damage, are defined depending on the stage of the disease and the degree of involvement. Pharmacological therapy includes non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, sulfasalazine, methotrexate, bisphosphonates, and immunomodulators 2,3.
The following is the case of an adolescent girl with CRMO detailing the diagnostic and therapeutic approaches used, as well as the positive response obtained after providing pharmacological treatment with NSAIDs and corticosteroids.
CASE PRESENTATION
A 16-year-old female adolescent in the tenth grade from Bogotá, Colombia, of mixed race and from a middle-income family, visited the emergency room of a quaternary care hospital of Bogotá in January 2019 due to a fever >38.5°, odynophagia, asthenia, and adynamia over the last two days. The patient, who had unintentionally lost 2kg in the previous month, was under medical observation due to a 1-year history of joint pain in the knees, the right ankle and metacarpophalangeal joints of the fourth and fifth fingers of the right hand, accompanied by episodes of erythema, edema, and flushing, especially in the right knee.
As a relevant medical history, the patient reported a bone biopsy in the right distal femur and proximal tibia 5 months before the date of admission; this study ruled out malignancy and showed morphological and structural changes compatible with osteomyelitis, although no microbiological isolation was performed. Based on these results, empirical antibiotic treatment with 300mg of clindamycin every 8 hours for 12 weeks was prescribed, which had already been completed at the time of admission to the emergency room.
In her anamnesis, the adolescent indicated that she had no pathological or traumatic history and reported that her parents were not consanguineous and had no relatives with autoimmune diseases. Physical examination revealed mucocutaneous pallor, skin without lesions, pain on palpation of the distal third of the right femur and pain on mobilization of the right knee, without other signs of local inflammation, no limitation in the mobility arches, and no joint effusion.
On admission to the emergency room, laboratory studies were carried out which yielded the following results: leukocytosis at 18 080 U/microliter (reference value (RV): 4 000-12 000 U/microliter), erythrocyte sedimentation rate (ESR) increased by 48 mm/h (negative value <15 mm/h), and slightly elevated C-reactive protein (CRP) at 10.5 mg/L (negative value <10 mg/L).
On the same day of admission, given the abnormal findings and the course of the disease, and because there was no clear diagnosis, the patient was admitted to the hospital to integrate and expand the studies that were available. At that time, the tests performed during the year prior to admission were also reviewed. As relevant findings, persistent elevation of CRP and ESR, leukocytes in normal ranges, and peripheral blood smear with the presence of microcytes were observed.
In addition, autoantibody studies (anti-Ro, anti-La, anti-RNP, anti-Sm, ANA, anti-DNA, and rheumatoid factor) were performed obtaining negative results, and some predisposing conditions for immunodeficiency, such as complement levels in blood, were ruled out: C3 in 105 mg/dL (RV: 86-206 mg/dL) and C4 in 24 mg/dL (RV: 8-55 mg/dL); and immunoglobulins: IgG in 1625 mg/dL (RV: 700-1600 mg/ dL) (IgM in 24 mg (RV: 40-230 mg/dL) and C4 in 226 mg/dL (RV: 70-400 mg/ dL); that is, the latter showed mild elevation of IgG, while IgM and IgA were in normal ranges. Human immunodeficiency virus infection was also ruled out.
During the first 3 days of hospitalization, hand and knee X-rays and a nuclear magnetic resonance imaging (MRI) of the lower limbs were performed. The right knee X-ray (Figure 1) showed no fractures, masses, lytic or sclerotic lesions and showed joint space preserved. However, comparative MRI of the legs (Figure 2) showed increased multifocal signal in distal femur and proximal tibia with osteopenia, no fractures, and a slight increase in joint fluid without involvement of articular cartilage and ligaments (according to the official report).
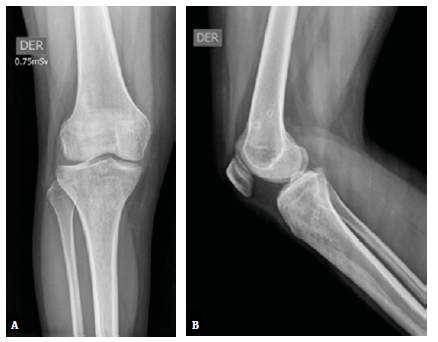
Source: Document obtained during the study.
Figure 1 X-ray of the right knee. A) anteroposterior view; B) lateral view.
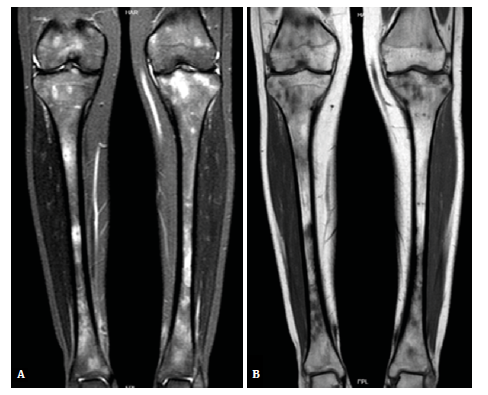
Source: Document obtained during the study.
Figure 2 Comparative nuclear MRI of the legs. A) STIR sequence; B) T1 weighted image.
It should be noted that, one month before admission to the emergency room, the patient underwent a bone scan that showed increased uptake in the left tibia and the metacarpal bones of the right hand, which could be related to multiple foci of osteomyelitis, as indicated in the official report.
On the sixth day of admission, based on intermittent episodes of joint pain, signs of local inflammation, persistence of elevated levels of inflammatory markers, imaging findings of multifocal bone lesions with inflammatory features, presence of sterile inflammation in histopathological study of bone, absence of evidence of neoplastic involvement, lack of microbiological isolation, and non-remission of symptoms after receiving a complete course of antibiotic management, a diagnosis of CRMO was considered.
Thus, once this diagnosis was contemplated and other diseases were ruled out, outpatient management with NSAIDs and corticosteroids was indicated to control symptoms. Therefore, after 6 days of hospitalization, the patient was discharged, and treatment was initiated with 250mg of naproxen every 12 hours and 25mg prednisolone daily (dose: 0.5 mg/kg/day).
Two months later, at a follow-up appointment with pediatric orthopedics, the patient, who was still on the same medical treatment prescribed at discharge, reported persistent episodes of joint pain and inflammation, although with less intensity and frequency. At that time, no local inflammatory changes or limitations in joint mobility were found, and no new studies were requested given the time elapsed since the last studies available and the favorable clinical course described. However, the importance of continuing multidisciplinary follow-up on a regular basis to define the need for adjusting treatment or implementing other interventions based on progress was emphasized.
DISCUSSION
According to the literature, several hypotheses have been established regarding the pathophysiological mechanisms of CRMO. For example, it has been suggested that dysregulation of the innate immune system leads to an imbalance between proinflammatory cytokines, such as interleukins (IL) IL-1p and IL-6 and tumor necrosis factor (TNF), and anti-inflammatory cytokines, such as interleukins IL-1β and IL-19 1-4, resulting in chronic inflammation associated with bone resorption and remodeling. This inflammatory process is caused by the modulation exerted by the cellular and humoral components of the immune system in the proliferation and differentiation of osteoclasts. Both processes are mediated by different signaling pathways, among which the one related to the receptor activator of nuclear factor kappa-β ligand (RANKL) stands out 5.
Other hypotheses suggest that it is a polygenic disease originating from the presence of sterile osteomyelitis in some syndromes and the increased frequency of individuals affected by this condition in some families 5,6. Monogenic disorders leading to the development of bone inflammation have also been described and explain some syndromic forms such as Majeed syndrome; pyogenic arthritis, pyoderma gangrenosum, and acne (PAPA) syndrome; and IL-1 p receptor antagonist deficiency 7,8.
CRMO usually presents with insidious bone pain, signs of local inflammation, fever, weight loss, and fatigue. The bones most commonly affected by this entity are the long bones of the lower limbs, especially the tibia, while the skull is the least affected. The duration of active disease varies from 2 to 5 years, but cases with longer periods of time have been reported 9-15. Furthermore, a strong association has been established between this disease and the presence of skin disorders (such as psoriasis and severe acne), inflammatory bowel diseases, and arthritis 16,17.
CRMO is diagnosed based on clinical and paraclinical parameters, including laboratory and imaging tests, as well as histopathological studies of the bone in many cases. However, there is no consensus to diagnose this disease, and although clinical criteria have been proposed for its operational definition, they have not been widely accepted or adopted. Moreover, there are no biomarkers or specific imaging or histopathological findings for this condition, so it remains an exclusion diagnosis 18,19.
Different groups of drugs are used to treat this disease, including NSAIDs, corticosteroids, sulfasalazine, methotrexate, bisphosphonates, anti-TNFα, and IL-1 receptor antagonists 20,21. It is important to note that the indications and regimes of the aforementioned drugs vary greatly 21.
NSAIDs are widely used in mild and moderate cases of CRMO and are useful in improving pain. More aggressive treatments including TNFa inhibitors or bisphosphonates should be considered in severe cases with inflammation of the vertebrae, structural damage, pathological fractures or damage to the physis 21,22. Nevertheless, the latter should be reserved for specific cases in which there is multifocal, mandibular or vertebral involvement, or the patient has diseases refractory to other drugs 21-23.
CRMO was diagnosed in this case after approximately 12 months of follow-up and multiple extension studies, which is consistent with what has been reported in the literature. According to some case studies, the average time between the onset of symptoms and considering this entity as the likely etiology is 15 to 18 months 23,24.
The fact that CRMO is an exclusion diagnosis can lead to the performance of multiple studies and procedures in short periods of time, as well as the administration of empirical treatments, with the resulting implications for patients and their families, which, when combined with the feelings generated by not having a clear diagnosis and no improvement in symptoms, affects the quality of life of those who suffer from this disease.
The patient in this case had a favorable response after starting combined management with NSAIDs and corticosteroids, which supports the usefulness of this therapy as reported in the literature. For example, Schultz et al., cited by Barral-Mena et al.25, described responses to NSAIDs in 79% of cases in a series of 190 patients without specifying the time of treatment or subsequent recurrences. In this regard, it is critical to conduct laboratory and imaging studies following the start of the indicated treatment in order to evaluate possible modifications in the parameters analyzed. However, in this case, due to the time of follow-up and the absence of signs or symptoms that could suggest disease progression or the appearance of complications, no new studies were carried out, which was a limiting factor for the overall analysis of the case.
Given this scenario, further research on the subject is needed to improve the available knowledge and thus achieve a real impact on outcomes in patients with CRMO. It is also necessary to resolve questions that arise on a daily basis, such as the frequency with which follow-up imaging studies are required, the impact of therapeutic interventions, the decrease in the variability of treatment schemes, remission rates, and individual conditions or findings that may correlate with prognosis and outcome for each patient.
CONCLUSIONS
CRMO, as well as other inflammatory diseases, should be considered in patients with intermittent bone pain of poorly defined course and accompanied by non-specific symptoms and signs. In this sense, it is necessary to integrate all available tools and initiate available treatments as soon as possible to control the disease and reduce the risk of progression and complications.
To date, little is known about CRMO, so it is essential to carry out new research to expand and deepen knowledge about it, which will allow issuing recommendations based on quality evidence.














