INTRODUCTION
Urinary tract injuries are the most common serious complication of laparoscopic pelvic surgery 1, and although their frequency varies depending on the gynecological surgery performed, Findleya & Solnik 2 found that between 0.2 and 15 cases occur per 1 000 procedures. Factors such as peritoneal adhesions, previous surgeries, and the presence of pelvic masses increase the risk of this type of injury.
Urinary tract injuries can be identified in the early or late postoperative period, and signs and symptoms include ileus, fever, anorexia, urinary ascites as a sign of cystotomy, and renal colic when there is ureteral obstruction 2.
The intrauterine device (IUD) is a small T-shaped plastic device used as a contraceptive method and can sometimes cause perforation of the uterus and migrate to pelvic or abdominal organs. The incidence of IUD migration and uterine perforation is reported in 1.9-3.6 cases per 1 000 insertions. It is worth mentioning that bladder perforation due to a displaced IUD is rare and is believed to occur primarily at the time of insertion. An IUD that migrated to the lower urinary tract, according to the literature, can be removed by three different methods: cystoscopy, laparoscopy, or open surgery 3.
In a 5-year retrospective cross-sectional analysis (January 2013 to December 2017) performed on 4 557 patients with IUD, Sharma & Suneja 4 found 71 cases of women (1.6%) requiring surgery for removing migrated devices, of which 63 (88.7%) were incomplete or embedded perforations and 8 (11%) were complete perforations or IUDs that migrated to omentum, vesicouterine pouch fundus, mesentery, or bladder.
Intraperitoneal bladder injuries require surgical repair 5, which is traditionally performed by laparotomy; however, little information is available on minimally invasive treatments in this clinical setting. The laparoscopic approach has demonstrated clear benefits, such as decreased bleeding, postoperative pain, intra-abdominal adhesions, risk of incisional hernias, and length of hospital stay and disability; improved visualization of pelvic organs; and early return to daily activities 1,5-7.
The following is the case of a patient who was successfully treated for intraperitoneal bladder injury secondary to gynecological pelvic surgery using a laparoscopic approach.
CASE PRESENTATION
A 39-year-old, mestizo, single woman from a low-income household and living in Bogotá (Colombia), was treated by the outpatient gynecology and obstetrics service of a tertiary care university hospital in Bogotá due to a 1-year history of moderate, intermittent, pressure-type abdominal pain predominantly in the left hypogastrium and iliac fossa. No other associated symptoms or significant medical or surgical history were reported, besides two pregnancies with vaginal birth.
Physical examination found that the patient had deep and superficial tenderness of the hypogastrium and right iliac fossa, although no signs of peritoneal irritation were observed. There was also pain on vaginal palpation of the anterior wall of the vagina and the left adnexa, with a sensation of mass and enlargement of the posterior cul-de-sac. During the consultation, the patient reported that an IUD that she had been using as a contraceptive method for the last five years had been removed seven months earlier in another hospital.
Based on the findings, she underwent an outpatient enhanced CT of the abdomen and pelvis, which revealed the presence of a hyperdense foreign body compatible with the presence of an IUD migrated to the left vesicouterine pouch, located outside the uterus, and in close contact with the posterior wall of the bladder. This indicated that the first attempt to withdraw the IUD was not successful.
Given the patient's symptoms, a left salpingectomy was performed via laparoscopic approach, resecting the migrated IUD. During this procedure, performed one month after the gynecological consultation, the presence of a copper IUD migrated and inserted into the left uterine horn and into the left round ligament with surrounding inflammatory changes was confirmed. No lesions were reported under direct vision in other abdominal or pelvic organs. The patient progressed satisfactorily and was discharged one day after surgery. It should be noted that during her hospital stay, she received postoperative analgesic management and no alarming signs were present.
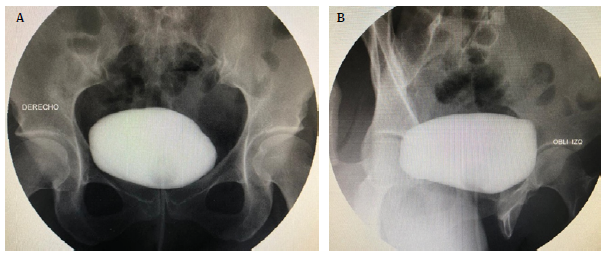
Three days after surgery, the patient visited again the emergency department of the same hospital due to anuria and generalized abdominal pain. On physical examination, vital signs were found within the normal ranges, and distension and moderate abdominal pain with no signs of peritoneal irritation were the only findings of relevance. Laboratory tests were performed, obtaining the following results: urinalysis with microhematuria, serum creatinine of 4.35mg/dL, and urea nitrogen of 35.2 mg/dL. Due to the suspicion of bladder injury, a urinary diversion with urethral catheter was passed to drain urine, and computed tomography (CT) cystography was requested. The procedure was performed on the day after readmission and showed a solution of continuity on the left posterolateral intra-peritoneal bladder with approximate dimensions of 14x13mm, through which the contrast medium was leaked into the peritoneal cavity (uroperitoneum) (Figure 1).
Source: Document obtained during the course of the study.
Figure 1 A) Sagittal view - CT cystography (arrow pointing to lesion site). B) Coronal-view - CT cystography (star indicating the presence of contrast medium in the peritoneal cavity).
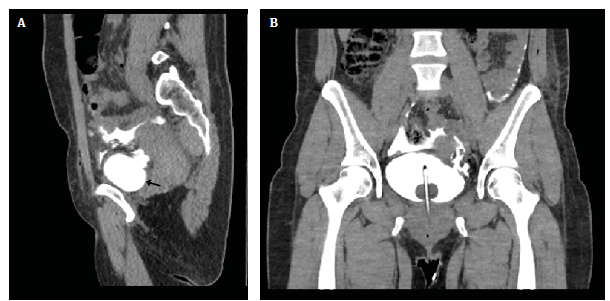
Based on the imaging findings, the patient was taken to emergency surgery two days after hospital readmission for transurethral cystoscopy and placement of 6Fr open-end bilateral ureteral catheter (bilateral endoscopic renoatmospheric stent), in addition to laparoscopic repair of the bladder injury. During these procedures, a fistula with irregular borders and approximately 2cm in diameter along its major axis was observed on the left posterolateral side of the bladder (Figure 2).
Source: Document obtained during the course of the study.
Figure 2 Endoscopic findings of transurethral cystoscopy. A) defect in the left posterolateral bladder wall; B) hydrophilic guidewire emerging from the left ureteral meatus.
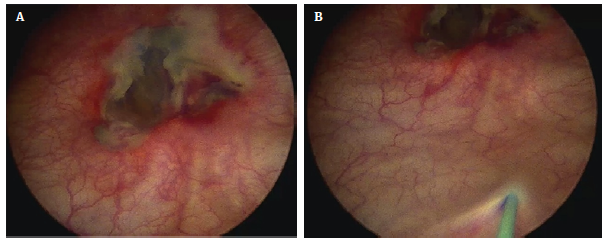
For the laparoscopic approach, four trocars were used and distributed as follows: a 12mm umbilical trocar, two 12mm trocars in both iliac fossa at the midclavicular line crossing, and a 5mm accessory trocar in the right iliac fossa. This approach allowed finding urine in the peritoneal cavity and confirming the presence of a defect with irregular borders on the left posterolateral side of the bladder (Figure 3).
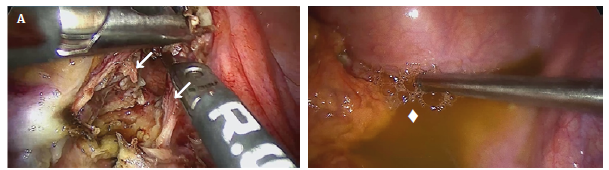
Source: Document obtained during the course of the study.
Figure 3 Laparoscopic findings. A) defect in the posterior wall of the bladder (arrows show the lateral edges of the bladder injury); B) uroperitoneum (star points to urine in the peritoneal cavity).
During this procedure, the devitalized edges of the bladder defect were also removed, and suturing was done in two planes with a 3-0 barbed suture, achieving an adequate and hermetic closure thanks to endoscopic and laparoscopic vision (Figure 4). Cystoscopy confirmed that the bladder defect had been properly closed and that the left urethral meatus was not involved. The 6Fr open end ureteral catheters were then threaded to the 16Fr Foley catheter and secured with 2-0 silk suture. The bilateral endoscopic renoatmospheric stent was maintained for one week and the urethral catheter for two weeks.
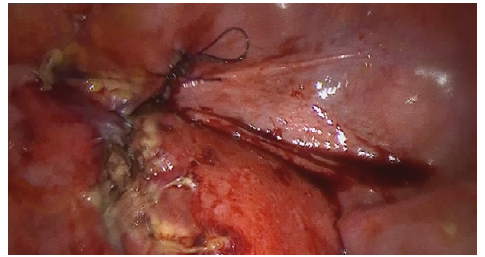
Source: Document obtained during the course of the study.
Figure 4 Laparoscopic view after closure of the bladder defect.
The patient had a satisfactory postoperative course and her blood creatinine levels improved, reaching values of 0.6mg/dL. Two days after the procedure, she was discharged and two weeks later a follow-up retrograde cystography was performed, confirming adequate resolution of the bladder injury (Figure 5) and the Foley catheter was removed without complications. After two months of outpatient follow-up, the patient was discharged by the urology service due to her good clinical course and the absence of urinary symptoms.
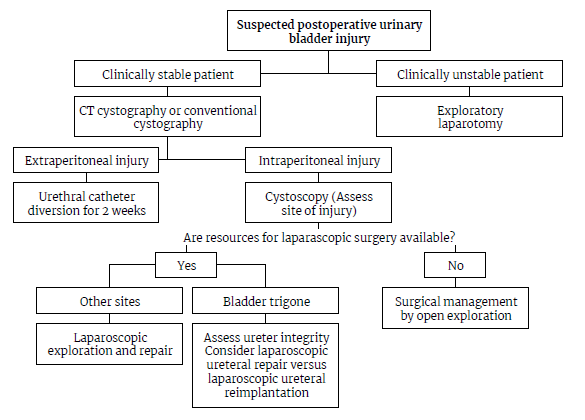
DISCUSSION
Since its introduction in the 1970s, the laparoscopic approach has proven to be one of the most significant advances in surgery 1, allowing for the completion of various procedures. For example, as stated by Aydin & Mercimek 7, in 1994, Parra reported the first laparoscopic repair of an intraperitoneal bladder perforation after iatrogenic bladder trauma.
Laparoscopy has demonstrated clear benefits, including reduced hospital stay, bleeding, postoperative pain, disability time, intra-abdominal adhesions, and risk of incisional hernias; early return to daily activities; and improved visualization of the pelvic organs 5-7.
When grouped, urinary tract injuries represent the most common type of major complications in laparoscopic pelvic surgery 1. Bladder injuries are caused by obstetric and gynecologic surgery, general surgery, and urological surgery in 65%, 22%, and 13% of cases, respectively 8.
The bladder is at risk of injury during gynecologic laparoscopic surgery for two reasons: the trocar insertion process, for example during suprapubic port placement, or its close relationship with the surgical field, such as during hysterectomy 1. Regarding laparoscopic pelvic surgery, the reported incidence of bladder perforation varies widely, with injury rates ranging from 0.02% to 8.3%, placing this injury at the top of the list of visceral complications 1.
Some of the risk factors for urinary tract injury during gynecological surgeries include a history of radiation or pelvic surgery, endometriosis, urinary tract anomalies, peritoneal adhesions, pelvic masses, obesity, and uterine fibroids, as well as the surgeon's lack of experience, specifically a low volume of laparoscopic gynecological surgical procedures performed 7.
Although not supported by evidence, performing bladder catheterization prior to peritoneal insufflation and trocar insertion is recommended as good clinical practice to avoid injury to a distended bladder 1,9. Preoperative prophylactic ureteral catheterization is debatable, as a beneficial effect on reducing the risk of ureteral injury during gynecological surgery has not been demonstrated consistently 7. Thus, to reduce the risk of urinary injury during gynecologic laparoscopic surgery, it is critical to understand and follow electrosurgery safety precautions, as bladder injuries may be difficult to detect because they can occur at a site distant from the surgeon's view and/or present as a late tissue rupture several days after the primary injury 1.
The following are some of the safety measures to consider for preventing potential complications related to electrosurgery in laparoscopy 1:
Carefully inspect instrument insulation with the anatomical structures of interest before using electrical power.
Use the lowest power setting possible to achieve the desired effect from the instruments.
Use a low-voltage waveform for monopolar diathermy.
Use bipolar energy when appropriate.
Use brief intermittent activation during surgery.
Do not activate instruments during laparoscopic surgery near or in direct contact with another instrument.
Make sure that forceps are always in sight of the surgeon when activating power instruments.
Signs and symptoms of bladder injury include macroscopic hematuria, abdominal or suprapubic tenderness, inability to urinate, and oliguria 1,6,8. These symptoms usually appear within the first 48 postoperative hours after sustaining a thermal injury or up to 10-14 days after the procedure 1. Biochemical profiles help diagnose this type of injury because serum creatinine levels rise abnormally due to its reabsorption into the urine through the peritoneal membrane 1, as was the case of the patient reported here.
When evaluating patients with suspected bladder injury, imaging studies, such as retrograde cystography or CT cystography, are necessary, since they have sensitivity and specificity of 95% and 100%, respectively 5,6.
Extraperitoneal bladder injuries can be treated conservatively with a bladder catheterization 1; however, intraperitoneal injuries require surgical repair 10 because, if untreated, they can lead to complications such as peritonitis and sepsis 5.
Traditionally, intraperitoneal bladder injuries have been treated with laparotomy 11, but current literature also describes cases of laparoscopic bladder repair, for example, following blunt abdominal trauma 6,12. Matsui et al.13, in a case report of a 61-year-old patient with acute abdomen secondary to intra- and extraperitoneal bladder injury, showed that laparoscopic repair may be indicated even in emergency situations involving bladder rupture.
An injury involving or near the bladder trigone carries the risk of urethral injury that can be assessed endoscopically 1. In most cases of bladder injury during laparoscopic surgery, repair should be performed by a urologist or gynecologist with advanced laparoscopic skills to avoid additional morbidity beyond that caused by laparotomy 1.
Cystotomy repair, i.e., surgical suture used to close a bladder injury, should be performed with absorbable suture to avoid creating a nidus that promotes the formation of urinary stones. It can also be performed with single-layer or two-layer technique, either continuous or interrupted 6. Urinary diversion with a Foley catheter for continuous drainage should be maintained for two weeks 1.
The case presented here describes the successful laparoscopic management of a bladder injury caused by gynecologic laparoscopic surgery in a tertiary care university hospital. Although the literature describing the laparoscopic management of post-surgical bladder injuries is scarce, the available evidence shows that the laparoscopic approach to injuries of this type, even those caused by blunt abdominal trauma, is feasible, has satisfactory outcomes, and is the current recommendation 6,14,15. Therefore, if the necessary resources (infrastructure, technology, human resources trained in laparoscopy, etc.) are available, the laparoscopic approach should be considered as the route of choice for the early management of iatrogenic bladder injuries in clinically stable patients (Figure 6).
CONCLUSION
This is the case report of a patient who had a bladder injury during the laparoscopic removal of an IUD that migrated to the uterine horn and vesicouterine pouch, which was diagnosed in the postoperative period and corrected via laparoscopy. Considering the advantages of laparoscopy over open surgery, and extrapolating the positive outcomes obtained with the laparoscopic management of traumatic bladder injuries in this patient, it is possible to conclude that the laparoscopic approach to surgical injuries in this organ should be regarded as a viable treatment option. Nevertheless, it is essential to keep in mind that this procedure requires assistance personnel with advanced laparoscopic training, as well as interdisciplinary support to provide comprehensive care to the patient.