INTRODUCTION
Takotsubo cardiomyopathy (TC) is a transient, reversible cardiac condition characterized by left ventricular systolic and diastolic dysfunction that is usually triggered by stress and can be easily mistaken for acute coronary syndrome. Complications associated with TC may be severe and include acute heart failure or even death 1.
TC recurrence is unusual because it occurs in less than 5% of cases, implying that there is insufficient data to suggest pathophysiological mechanisms or risk factors associated with this event 2. Additionally, the most effective treatment at the onset of a new episode is unknown, and no standard protocol of care exists to date.
CASE PRESENTATION
A 56-year-old middle-class mestizo housewife from Bogotá, Colombia, went to the emergency department of a tertiary care university hospital after experiencing for 24 hours symptoms of oppressive chest pain in the retrosternal space associated with physical activity that improved partially with rest. The patient stated that her symptoms appeared 4 hours after a stressful emotional event and that she had dyspnea, diaphoresis, and edema in the lower limbs.
Relevant medical history included arterial hypertension and hypothyroidism. The patient also reported that 4 years earlier she had an episode of TC (diagnosed by ventriculogram) that resolved without the use of a ventricular support device. She also reported that she was taking losartan 50mg every 12 hours, metoprolol 50mg per day, aspirin 100mg per day, and levothyroxine 75mg per day on an outpatient basis, and that she had not developed any other symptoms before the consultation. The patient was classified as functional class I according to the New York Heart Association classification of heart failure.
When the patient had her first episode of TC 4 years earlier, a coronary angiogram was performed, ruling out coronary lesions and identifying an emotional stressful event related to the death of a relative. In addition, an echocardiogram performed one year prior to admission revealed no segmental alterations in contractility and a left ventricular ejection fraction (LVEF) of 56%.
On admission examination, the patient had the following vital signs: blood pressure: 155/80 mmHg, heart rate: 98 bpm, respiratory rate: 18 rpm, and arterial oxygen saturation: 91% on room air. Physical examination was normal.
In the first hour of admission, the patient underwent an electrocardiogram (Figure 1) that showed alterations due to sinus tachycardia and T-wave inversion in leads V1-V4, without ST segment alterations, and normal QTc values. On admission, troponin I was 500 pg/mL (reference: range: 0-15.6 pg/mL), and a subsequent test (taken 3 hours later) yielded a value of 1127 pg/mL.
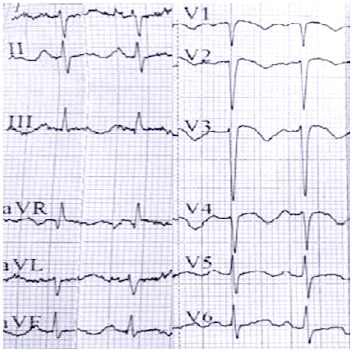
Source: Own elaboration.
Figure 1 12-lead electrocardiogram showing sinus tachycardia associated with repolarization abnormality in leads V1-V4 and QTc interval prolongation.
Based on the findings, a possible non-ST-segment elevation acute myocardial infarction was considered, with a cardiovascular risk stratification of 87 on the GRACE scale and 3 on the TIMI scale. Treatment was started with aspirin 100mg, clopidogrel 75mg (prior loading of 300mg of aspirin and 300mg of clopidogrel), atorvastatin 80mg, enalapril 5mg, metoprolol 50mg, and enoxaparin 60mg, drugs that were administered every 12 hours.
The echocardiogram performed on the same day of admission (Figure 2) also showed moderate left ventricular dysfunction with a LVEF of 38% associated with apical dyskinesia, involving akinesia of the mid-distal segments of the anterior wall, distal to the inferior wall, mid-distal to the lateral wall, and distal to the posterior interventricular septum, findings suggestive of apical ballooning. No right ventricular dysfunction was reported, and pulmonary artery systolic pressure was 60 mmHg, which was associated with mild tricuspid valve regurgitation.
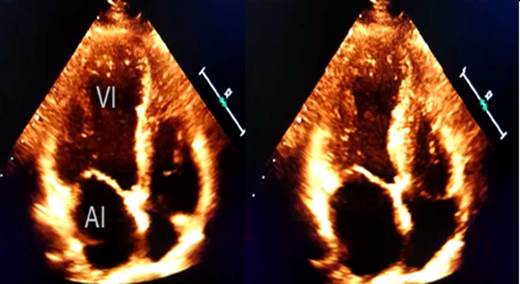
Source: Own elaboration.
Figure 2 Echocardiogram in apical four-chamber view during the phases of diastole and systole. AI: left atrium; VI: left ventricle.
On the same day of admission, the patient was admitted to the cardiovascular care unit and a coronary angiogram was performed, which showed no significant lesions in the epicardial coronary arteries; in addition, apical ballooning was evident in the ventriculogram (Figure 3).
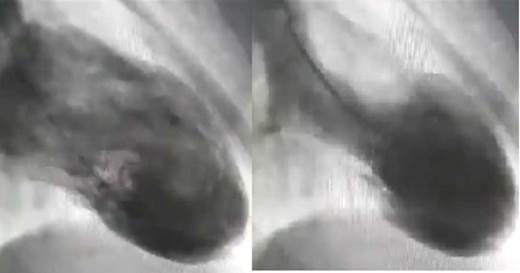
Source: Own elaboration.
Figure 3 Ventriculogram in diastole and systole with image suggestive of apical ballooning.
Given the pattern of echocardiographic and angiographic involvement and the absence of coronary artery disease in the patient, recurrent MT was suspected, thus clopidogrel and aspirin were discontinued and metoprolol and enalapril were administered at the same doses, with no adverse effects. Since the patient remained asymptomatic and had no new episodes of chest pain, she was discharged after four days of hospitalization.
A follow-up echocardiogram, performed 8 weeks after admission, showed an LVEF of 52% and no evidence of segmental contractility disorders. The patient did not report any associated symptoms during this last visit.
DISCUSSION
TC is also known as Takotsubo syndrome, apical ballooning syndrome, stress cardiomyopathy, broken heart syndrome, among others. The term Takotsubo is a Japanese word that describes a vessel used to catch octopuses, which is characterized by a thin neck and a round base. This image is similar to that observed on ventriculogram in right oblique projection during systole of patients with this alteration; however, other patterns of involvement have been described, with apical involvement being the most frequent (81.7%), followed by the mid-ventricular variant (14.6%), the basal form (2.2%), and the focal form (1.5%) 1. The patient in this case presented with the apical variant.
The incidence and prevalence of TC has increased in the last 20 years, and it is considered that approximately 2% of patients taken to coronary angiography for suspected acute coronary syndrome actually have a TC 3,4.
Traditionally, TC has been considered a benign condition 5; however, significant alterations in myocardial perfusion have been observed 6, and mortality in the acute presentation is estimated to be about 5% 7.
Several theories have been proposed to explain the pathophysiology of TC, which have established that there are several factors that can modify its onset and presentation 8. Nevertheless, its etiological mechanism has not been elucidated, although, taking into account the occurrence of TC in twins, it has been suggested that there may be a genetic component. Moreover, studies in animal models have determined the relationship between the overexpression of genes related to the physiological response to stress and the appearance of this disorder, with particular emphasis on the overexpression of genes encoding adrenergic receptors 9.
The difference in adrenergic receptor density along the myocardium could explain the anatomical patterns of presentation of TC, with beta-2 adrenergic receptors being widely expressed in apical regions, whereas beta-1 receptors for norepinephrine have a predominantly basal distribution and are related to catecholamine levels that could induce myocardial injury associated with coronary artery spasm 9-11. This combines with an increase in ventricular afterload induced by sympathetic overstimulation, which eventually favors cardiac injury.
Recent data suggest that, in patients with sepsis, the associated presentation of TC is reflected in a significant reduction of in-hospital mortality. This could suggest cardioprotective mechanisms during sympathetic stress and would allow establishing the hypothesis that a certain percentage of sepsis-induced cardiomyopathy cases could be explained by this pathophysiological mechanism 10,11. It is estimated that about 90% of cases of TC occur in postmenopausal women, as in the case reported here, suggesting a possible protective effect of estrogens 3,12.
TC recurrence has been documented since it was recognized as an independent entity, but there are few related data. For example, Singh et al.2, in a systematic review that included 31 cohort studies with 1 664 patients, found 74 cases of recurrence (4.4%) with a mean follow-up of 24.5 months, but were only able to establish adequate follow-up data for 23 of these patients. They also estimated that the cumulative incidence of recurrence was approximately 5% at 6 years and that the annual recurrence rate was about 1.5%. Moreover, these authors found that 14% of patients presented chest pain as a recurrent symptom, which also occurred in the patient in this case, and that 11% reported dyspnea without definitive evidence of recurrent TC 2.
Furthermore, the study by Singh et al.2 emphasizes that the recurrence rate was higher in patients who had a higher degree of ventricular dysfunction in the first episode, suggesting that these patients may have an increased susceptibility that could be a predictor of recurrence. This study also established that the majority of patients with recurrent TC were women and that the stressful event might be different from that reported during the first episode, which is consistent with what was found in the case presented here 2.
Persistent ST-segment elevation, defined as elevation for at least 48 hours, has been described in about 20% of patients with TC and has been associated with increased hospitalization stays and/or in-hospital complications. This fact has also been proposed as an independent factor for future major cardiovascular episodes after discharge 13.
In a study of 749 patients with TC from 9 European centers that are part of the GEIST registry, El-Battrawy et al.14 identified a mean recurrence rate of 4% at 830 days and established that baseline characteristics among patients with recurrence or who had their first episode did not differ; however, the presence of pulmonary edema was greater in the recurrence group.
In another retrospective study evaluating echocardiographic characteristics of 114 patients with TC, El-Battrawy et al.15 found a recurrence rate of 6.1% and reported a statistically significant relationship between recurrence episodes and the presence of arterial or pulmonary hypertension, and that echocardiographic presentation could vary in patients showing segmental involvement other than the index event. For this reason, there is a discrepancy with the theory related to the distribution of beta-adrenergic receptors in the myocardium. In this regard, Xu et al.16 suggest that the foregoing may be a result of myocardial conditioning that prevents involvement of previously involved areas. Concerning this latter remark, it should be mentioned that in the case described here, the segmental distribution of the first episode is not known.
In a multivariate analysis, Lau et al.17 found that the risk factors associated with recurrence of TC or death from this cause were age (HR: 1.56; 95%CI: 1.291.87 for each additional 10 years), male sex (HR: 2.52; 95%CI: 1.38-4.60), diabetes (HR: 1.6; 95%CI: 1.06-2.43), pulmonary disease (HR: 2.0; 95%CI: 1.37-2.91), and chronic kidney disease (HR: 1.58; 95%CI: 1.01-2.47).
TC is characterized by widespread myocardial edema, which appears in the acute phase, can persist for up to 4 months, and can be easily identified in a cardiac magnetic resonance, which also adequately describes ventricular function, especially in T2 weighted sequences. Furthermore, the use of delayed gadolinium enhancement in this imaging test allows the identification of ischemic heart disease and myocarditis, but this finding is not usually observed in TC cases 18.
Interventions implemented to prevent TC recurrence include therapy with beta-blockers, ACE inhibitors, and angiotensin II receptor blockers (ARBs), among others. To date, however, there is no clear evidence to establish that one therapy is more effective than the other.
From a pathophysiological approach, the use of beta-blockers sounds reasonable considering that they are drugs that can intervene in the abnormal response to stress-induced catecholamines. In spite of this, in a meta-analysis, Santoro et al.19 failed to establish an association between the use of beta-blockers, ACE inhibitors, ARBs, or statins and the effective reduction in recurrence rates. In addition, Singh et al.2 were also unable to demonstrate a relationship between the use of beta-blockers and ACE inhibitors and a decrease in recurrence rates.
Similarly, according to Santoro et al.19, aspirin does not seem to confer a protective effect in terms of recurrence either, but Brunetti et al.20, in a later analysis, suggested a possible benefit of the use of combined therapy.
In the present case, differential diagnoses could be ruled out using coronary angiogram, and the patient could be followed up on to confirm the recovery of ventricular function. Nonetheless, it should be noted that adequate data on the first TC episode were not available, and adherence to the therapy implemented at that time is unknown.
Given the lack of evidence on the management of TC, and based on the possible related pathophysiological mechanisms, its treatment remains empirical.
The present case demonstrates the possibility of TC recurrence and confirms that it is feasible to regain cardiac function following appropriate therapy.
CONCLUSION
TC is a condition with increasing prevalence and recurrence is a rare complication. The description of this case report is intended to raise awareness among clinicians of the possibility of recurrence of this syndrome so that appropriate treatment can be implemented. However, clinical trials are needed to adequately evaluate therapies that reduce the risk of recurrence given the likelihood of adverse cardiovascular outcomes related to recurrence.














