INTRODUCTION
Hydatidosis, also known as cystic echinococcosis, is a parasitic disease caused by the larval form of the cestode Echinococcus granulosus and is currently classified as the main endemic zoonosis in Chile, with notification rates ranging from 1.4 to 2.47 cases per 100 000 inhabitants between 2000 and 2014. This disease is also predominant in livestock areas such as the southern part of the country 1.
This disease manifests as a cystic lesion consisting of an endocyst or germinal membrane (containing scolices, daughter vesicles, and hydatid fluid) and a pericyst or exocyst, composed of inflammatory or fibrous tissue from the host 2. Hydatid cysts are found mainly in the liver (70%), followed by the lungs (20%) and various regions such as brain, spleen, kidneys or heart 3. Similarly, it has been established that 1-5% of cases occur in musculoskeletal tissues 4, with the pelvis being the second most involved bone (21%) 5,6.
The spread of hydatidosis is explained by the difference in size of 20 microns in the portal vessels, 8 microns in the pulmonary vessels, and 30-36 microns in the oncosphere (larval form of cestodes), being these organs the main filters for the development of the disease; however, they can occur in other systems if barriers are overcome 4.
Hydatidosis is generally diagnosed at 40 years of age in men and at 36 of age years in women 1 and is characterized by a slow cystic growth in musculoskeletal tissues that can eventually lead to neurological manifestations, pathological fractures, hemorrhages, deep vein thrombosis, among others 6.
The aim of this study was to present an atypical form of hydatidosis, as well as to review relevant elements associated with it and its treatment, since there is no consensus on the standard management of this disease in atypical non-visceral locations.
CASE PRESENTATION
A 41-year-old woman with no relevant medical or surgical history, who worked as a waitress, lived in the urban area of southern Chile at a low-income household. She went to the emergency room of the Hospital Base San José de Osorno, Chile, due to lumbosacral pain radiating to her left thigh for a week following a fall.
On admission, the patient's hemodynamic status was stable, without fever or a history of weight loss. Physical examination revealed pain on palpation of the lumbosacral joint and on the left side of the hip when it was flexed. During the directed anamnesis, the woman denied ownership of dogs and reported no history of hydatidosis in her family. However, she reported frequenting a rural area where cattle were raised for human consumption. After the initial assessment, an anteroposterior pelvic X-ray was performed, which showed no acute bone injury. Likewise, a computed tomography (CT) scan of the abdomen and pelvis was performed without enhancement, which showed a mass with erosive bone destruction in the iliac bone, so she was admitted to the hospital for treatment by the surgery service.
On the same day of admission, during hospitalization, an enhanced CT scan of the chest, abdomen and pelvis was performed, which showed a heterogeneous pelvic tumor involving the left iliopsoas muscle that was lobulated and measured 9.9x5.5cm. A second tumor of difficult delimitation and extending into the gluteal areas was observed in the left pyramidalis muscle (Figure 1). No pathological findings were identified in the liver, lungs, or other organs. Laboratory tests performed on admission showed leukocytosis of 17.5x103/UL with predominantly increased eosinophils (8.7x103/UL); other tests (red blood cell count, platelet count, tumor markers (alpha fetoprotein, LDH, β-hCG, Ca-125), and liver and kidney function were normal. Imaging studies showed no involvement of other organs.
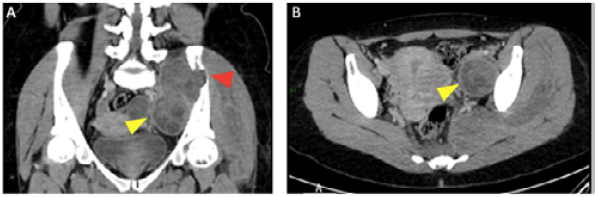
Yellow arrowhead: cystic lesion; Red arrowhead: bone involvement.
Source: Imaging scans obtained during the study.
Figure 1 A) Enhanced CT scan of the abdomen and pelvis (coronal plane); B) Enhanced CT scan of the pelvis (axial plane).
Given the findings, it was suspected that the disease had an infectious inflammatory etiology due to an atypical germ (mycobacteria, fungal or parasitic) or a neoplastic origin (lymphoma or sarcoma).
During hospitalization, the patient was evaluated by the hip surgery service and the oncology surgery team, who ordered a preperitoneal incisional biopsy, which was performed on the third day of hospitalization. In the course of this procedure, an abscessed cystic lesion containing hydatid membranes was identified, so a partial pericystectomy was performed with placement of drainage to the residual cavity.
The biopsy findings were consistent with hydatid cyst, and microscopy showed fibroadipose connective tissue adventitia and numerous scolices with signs of involution, which allowed establishing the diagnosis of hydatidosis. The patient was discharged on the fifth postoperative day and continued to receive outpatient treatment with albendazole 400mg every 12 hours for 12 weeks; at the end of this treatment, she had a slight increase in transaminase levels, which later normalized.
After discharge, the patient underwent check-ups every three months and a year later, a follow-up CT scan showed a cystic lesion in close contact with the left iliac wing and a collection partially surrounding the femoral vessels (Figure 2A), findings compatible with recurrence of the disease. On the same day, the woman was admitted, and intravenous treatment was started with ceftriaxone 1g every 12 hours and metronidazole 500mg every 8 hours, and a new surgery was scheduled to be performed on the fifth day of hospitalization. During the procedure, a large retroperitoneal hydatid cyst of approximately 10cm was observed, and the external iliac vein was found to be firmly surrounding the cyst. Therefore, partial pericystectomy was performed in approximately 70% of the area, leaving a patch of the cyst firmly attached to the iliac vein (Figure 2B). On the third postoperative day, the patient was discharged and continued with antibiotic treatment with amoxicillin/clavulanic acid 875/125mg every 12 hours until completing 14 days. Furthermore, treatment with albendazole 400mg was initiated every 12 hours for 8 weeks, which was well tolerated.
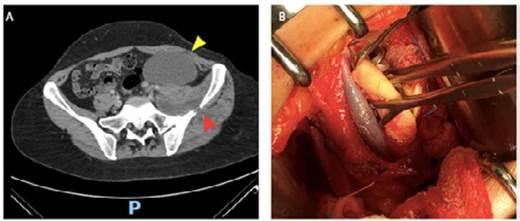
Yellow arrowhead: cystic lesion; red arrowhead: iliac bone destruction.
Source: Imaging scans obtained during the study.
Figure 2 A) CT scan of the pelvis (coronal plane); B) Extraction of hydatid membranes and iliac vein surrounding the cyst.
Two months after the second surgery, the patient presented with general malaise, febrile sensation, and purulent exudate in the operative wound, so she attended the emergency department again. On admission, laboratory tests showed leukocytosis of 11.3x103/UL and C-reactive protein levels of 169.5 mg/L. An enhanced CT scan of the abdomen and pelvis was also requested, showing a complex retroperitoneal cystic lesion of 5x6 cm consistent with disease recurrence (Figure 3).
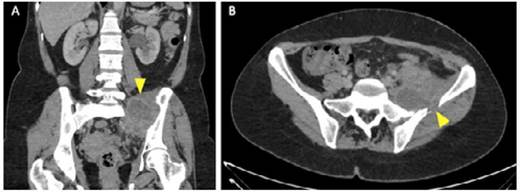
Yellow arrowhead: complex cystic lesion involving sacroiliac joint and iliac bone.
Source: Imaging scans obtained during the study.
Figure 3 CT scan of the abdomen and pelvis. Coronal plane (A) and axial plane (B).
The patient was hospitalized once again and received intravenous antibiotic treatment with ceftriaxone 1g every 12 hours and metronidazole 500mg every 12 hours. After a joint evaluation with the trauma service, it was decided to opt for a combined surgical treatment. Thus, the patient was taken to surgery on the fifth day of hospitalization and during the procedure a fistula with purulent contents (from the retroperitoneum to the skin) was observed.
A combined preperitoneal approach was used behind the iliac muscle, identifying an osteolytic lesion in the iliac bone with traces of whitish membranous tissue. Fistulectomy, surgical procedures, curettage of the iliac and sacral bone where the purulent collection was located, biopsy collection, and bone culture were performed.
The biopsy confirmed the presence of hydatid membranes with dense fibroconnective tissue and a non-specific chronic inflammatory process. Bone culture was positive for cloxacillin-sensitive Staphylococcus aureus, so intravenous antibiotic treatment was started with cloxacillin 2g every 6 hours and albendazole 400mg every 12 hours orally. The patient completed 4 weeks of treatment and was discharged with outpatient treatment for 8 weeks with oral sulfamethoxazole/ trimethoprim 800/160mg 2 tablets every 12 hours and albendazole 400mg every 12 hours. A total of 12 weeks of antiparasitic treatment was well tolerated and allowed controlling the infection.
The patient continued to be followed up on an outpatient basis by the surgery and infectious diseases services, and during a follow-up carried out 7 months after the last surgery, she was in good general condition and had no imaging or laboratory signs of disease recurrence.
DISCUSSION
The present case exposes two important elements to consider when dealing with retroperitoneal tumors: the complexity of the preoperative etiological diagnosis and the use of radical surgery with a multidisciplinary team for definitive treatment when dealing with atypical hydatidosis.
Extrahepatic or extrapulmonary hydatid cysts are an uncommon presentation of hydatidosis that account for less than 10% of all cases of this disease; however, it is not clear what percentage is associated with primary or secondary infection due to involvement of another organ 5,6. He et al.7 published a series of 1 257 cases of hydatidosis, in which 121 (9.6%) had retroperitoneal involvement (of which 68 were surgically treated) and, of these, only 4 (0.3%) had primary localization.
The isolated pelvic location of hydatidosis, being a rare form of presentation, requires a high index of suspicion, so it is critical to consider this disease in the differential diagnoses of musculoskeletal and/or retroperitoneal tumors. Pelvic lesions can range from purely cystic lesions to lesions with a predominant solid component. Retroperitoneum is a rare location for tumor lesions and their timely identification is critical since more than 80% of these tumors are malignant and usually large before they compress neighboring structures and cause symptoms 8. Therefore, when faced with a cystic lesion, hydatidosis should always be suspected, especially in regions of high prevalence such as southern Chile 1,8,9.
In order to establish the diagnosis of hydatidosis, a history of risk factors must first be collected, among which the most significant ones are living in endemic areas or in rural areas, owning dogs that have access to waste or that are fed with livestock viscera; having contact with livestock; consuming cattle slaughtered at home or in non-certified places; and having a family history of hydatidosis 1,9,10. The patient reported here stated that she frequented a rural area where cattle were raised for human consumption, which, as already stated, is considered a risk factor.
Regarding symptoms, hydatidosis is characterized by pain (56%), neurological deficit (37%), volume increase (9%), and complications such as bacterial superinfection, pathological bone fractures, bleeding, or venous thrombosis 6. In the case described here, the patient presented with pain, which was the reason for consultation, as well as bone destruction.
There are various laboratory studies that confirm the diagnosis of hydatidosis, the most commonly used being the ELISA test and indirect hemagglutination, which have a sensitivity of 98% and 85%, respectively 11. However, it is important to bear in mind that seronegativity is reported in up to 20% of cases with hydatidosis in the liver, as well as persistence of seropositivity for up to 10 years after treatment of the disease 12. No studies showing the performance of these tests in atypical locations were found in the literature review conducted for the preparation of this case report.
Preoperative biopsy or fine-needle aspiration are alternatives that may aid in the diagnosis of retroperitoneal tumor lesion 13; however, these procedures are not risk-free and are contraindicated against the suspicion of hydatid cysts given the risk of dissemination or anaphylactic shock 14. In the case presented here, surgical biopsy was chosen based on diagnostic suspicion and because of the technical difficulty associated with the proximity of vascular structures.
In cases of retroperitoneal hydatidosis, even with the various tools currently available, it is difficult to differentiate between malignant or benign lesions in the preoperative period and there are no proven algorithms for its management. Consequently, the study of this type of lesion is a complex task 13 and the diagnosis is often made intraoperatively 7, as in the case presented.
Concerning imaging, ultrasound is the cornerstone in the initial diagnostic approach to hydatidosis, but it should be noted that there is not much research comparing this study with other assessment methods. Stojkovic et al.15, in a retrospective study of hydatidosis, mainly in the liver, compared the use of ultrasound, CT scan, and magnetic resonance imaging and concluded that ultrasound is the main diagnostic method, but if the location of the cyst does not allow adequate visualization, MRI should be selected over CT. In the case presented, a CT scan was performed, given its availability in the emergency department.
If musculoskeletal hydatidosis is suspected, hepatic or pulmonary visceral involvement must first be ruled out. For this purpose, CT with intravenous contrast is very useful, as it allows defining the atypical location of the cyst and identifying the involvement of neighboring organs. Similarly, certain tomographic findings may guide the diagnosis of hydatidosis, such as the presence of a spherical or oval cyst with daughter vesicles inside and total or partial wall calcification; however, the findings are not pathognomonic and may simulate a soft tissue tumor or metastasis, requiring a histological diagnosis 16.
Chen et al.17 published a study describing the main tomographic features of pelvic hydatid cysts and established that CT detects some degree of bone reaction such as thinning of the bone cortex; expansive, osteolytic, or erosive bone destruction; invasion of soft tissues, mainly in the psoas muscle; and different calcification patterns of the cyst itself. In the present case, the CT scan showed erosive bone destruction resulting from the presence of a retroperitoneal pelvic mass.
Hydatidosis can be difficult to treat, as evidenced by Steinmetz et al.18, who conducted a literature review that included 200 publications with 721 cases of bone echinococcosis and found that 17% had a recurrence within a 2-year period.
Adjuvant treatment with drugs of the benzimidazoles family in the pre- and post-operative period is recommended by several authors 19,20; however, there is insufficient evidence to support its use. Thus, it is not recommended to administer these drugs in the preoperative period if the imaging diagnosis is uncertain, given that a biopsy or aspiration puncture would be contraindicated and that incorrectly treating a malignant lesion could worsen the prognosis of the patient.
García-Álvarez et al.20 published a series of 13 cases of musculoskeletal hydatidosis in which they found that the use of benzimidazoles did not improve the outcome in patients with bone involvement or with partial pericystectomy and that they had to be reoperated on. In the present case, the diagnosis was not certain in the preoperative period, so no treatment was administered and albendazole was indicated after surgery, although this did not prevent recurrence.
There are no studies comparing radical and conservative surgical treatment in musculoskeletal hydatidosis. However, García-Álvarez et al.20 showed that better results are achieved with radical resection, especially in patients with bone involvement who had to be reoperated on to complete bone resection. These authors also stated that resection of pelvic bones can be complex and safety margins are difficult to define, as the spread of hydatid disease in bones is not clearly described yet.
In cases of hydatidosis with a typical location, such as the liver, radical resection has been shown to be beneficial. Pang et al.21 conducted a meta-analysis on hepatic hydatidosis in which they found that radical surgery has less recurrence and morbidity than conservative surgery. However, there is not enough literature to support this, and despite the good outcome obtained in the present case it is difficult to extrapolate this position, so each case must be evaluated individually.
In the present case, the imaging study revealed a solid cystic tumor, and further study by surgical biopsy made it possible to make the diagnosis of hydatidosis. Similarly, a partial pericystectomy was performed, but the patient had a recurrence of the disease approximately one year later. A multidisciplinary approach that directed prolonged antibiotic management and a radical approach to the lesion resulted in adequate control of the disease.
CONCLUSION
High suspicion of parasitic diseases is important when dealing with retroperitoneal lesions with eosinophilia and altered serology. Multidisciplinary management of musculoskeletal hydatidosis is essential for achieving radical surgical treatment, which is the best option in complex cases and allows for good disease control while reducing complications and/or recurrences.














