INTRODUCTION
Gestational trophoblastic disease (GTD) is a term that refers to a group of rare gestational diseases caused by trophoblast proliferation in which the mechanisms controlling tissue invasion are altered 1.
Hydatidiform mole, also known as molar pregnancy, is a type of GTD that results from the abnormal fertilization of an oocyte. Its prevalence varies from 1 case per 500 to 1 case per 1 000 pregnancies depending on geographic location. Thus, in Asia and Latin America, its incidence is higher than in Europe and North America, and its frequency is twice as high in Asian women compared to Caucasian women 1,2. This complication may be classified as partial or complete. The former is characterized by the presence of embryonic or fetal tissue, together with a mixture of normal and abnormal trophoblastic villi. In this kind of hydatidiform mole there is genetic material from the mother in the mixture and, in most cases, it shows a triploid karyotype, thus differentiating it from the complete hydatid-iform mole, where there is no embryonic tissue and the karyotype is usually diploid and exclusively of paternal origin 2.
Vaginal bleeding is the most common clinical sign in patients with this condition, but nonspecific symptoms and/or signs such as abdominal pain or emesis may also be observed. Similarly, because patients with molar pregnancy have elevated levels of human chorionic gonadotropin (hCG), in some cases, pregnancy symptoms such as hyperemesis gravidarum or enlarged uterus may occur earlier than expected. Other typical clinical manifestations include anemia, acute respiratory distress syndrome, and hyperthyroidism, the latter two caused by the hormonal effect of elevated hCG levels on other organs 1.
Since vaginal bleeding is also one of the most frequent reasons for consultation in obstetric emergencies, a complete anamnesis and a comprehensive physical examination are essential, as they will allow suspecting the presence of hydatidiform mole as a differential diagnosis of first-trimester metrorrhagia 3.
Hydatidiform mole is considered a localized disease with a good prognosis if detected early and treated promptly. Although it usually resolves with surgical evacuation of the uterus, it may cause persistent trophoblastic disease 2. Therefore, in cases of hydatidiform mole, a good diagnostic approach that facilitates treatment is critical, as it limits invasiveness and improves the patient's prognosis.
CASE PRESENTATION
A 47-year-old housewife from a low-income household, from Morocco and of Berber ethnicity, attended the emergency department of the Hospital Clínico Universitario de Valladolid after a month of persistent coughing and emesis. At the consultation, she reported episodes of epigastralgia and amenorrhea for two months, as well as scant metrorrhagia in the previous 48 hours. Regarding obstetric history, the patient reported a euthyroid delivery 18 years prior to consultation.
On admission, a physical examination revealed a uterus that was not painful on palpation but was enlarged, with the fundus located in the umbilical region, a finding consistent with 20 weeks of amenorrhea. There were also traces of blood in the vagina, an erythroplastic cervix painful on movement, and a soft mass in the rectouterine pouch (also known as pouch of Douglas). Subsequently, a transvaginal ultrasound revealed a heterogeneous intrauterine mass measuring 124x120mm, as well as a small amount of free fluid in the rectouterine pouch; no adnexa were observed. A Doppler ultrasound was also performed, with no abnormal findings reported. Finally, an abdominal ultrasound showed a solid tumor inside the uterus that was 11 cm in diameter with a cystic, heterogeneous, and irregular appearance.
Moreover, the patient tested positive for pregnancy and the following results were obtained in laboratory tests performed in the emergency department: hemoglobin: 9.1g/dL, hematocrit: 26%, leukocytes: 6590/μL (73% neutrophils), and β-human chorionic gonadotropin (βhCG): 772 110 mIU/mL.
Given the diagnostic suspicion of an intrauterine tumor compatible with hydatidiform mole, it was decided to admit the patient to the hospital. During the first hours of hospitalization, a chest X-ray was performed, in which no abnormal findings were observed, as well as thyroid function tests (TSH: 0.01 IU/mL and T4: 6.34 ng/dL) and a blood test for Rh factor (A Rh -).
Once informed of the suspected diagnosis and the possible therapeutic options available (curettage or total hysterectomy), the patient decided to undergo a total hysterectomy because, as she stated, she had already fulfilled her desire to be a mother. Thus, 24 hours after admission, a total hysterectomy was performed by laparotomy with bilateral salpingectomy; there were no complications during the procedure, and a surgical specimen was obtained consisting of an enlarged uterus with a smooth surface (Figure 1) and a dilated endometrial cavity containing decidua, abundant vesicles, and grouped villi (Figures 2 and 3).

Source: Image obtained during the study.
Figure 1 Surgical specimen obtained during hysterectomy: enlarged uterus with a smooth surface.

Source: Image obtained during the study.
Figure 2 Macroscopic pathological findings contained in the uterine cavity and covered by decidua.

Source: Image obtained during the study.
Figure 3 Macroscopic pathological vesicles and villi found within the uterine cavity.
Follow-up examinations performed 48 hours after the procedure documented a ßhCG level of 102 800 mIU/mL. In view of the favorable postoperative course of the patient, the cessation of vaginal bleeding, and a last follow-up examination (βhCG level: 38 647 mIU/mL), it was decided to discharge her 72 hours after surgery with the indication to perform three weekly follow-up examinations, in which the following ßhCG levels were reported: 14 881 mIU/mL, 3 574 mIU/mL, and 2 004 mIU/mL, respectively. Subsequent monthly follow-up tests evidenced a progressive decrease in serum ßhCG levels until they were negative at 6 months. In addition, the patient progressively recovered from the sequelae of the surgery and reported no adverse effects.
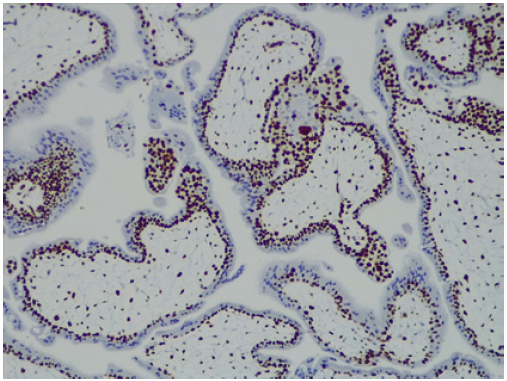
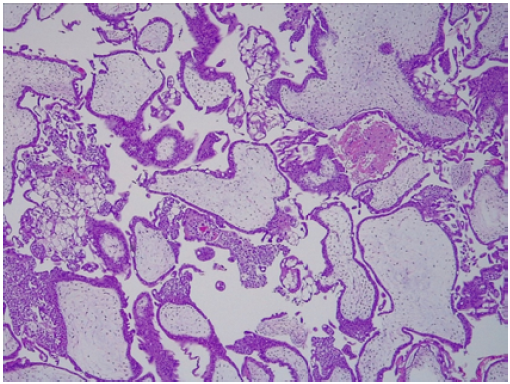
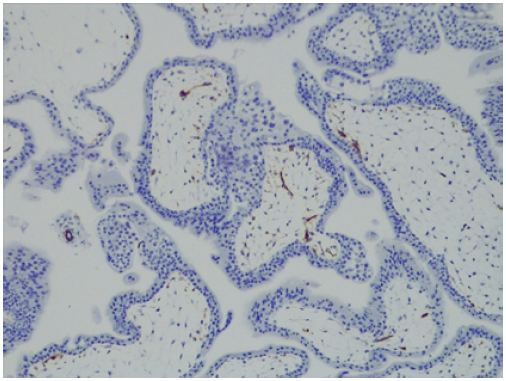
The pathology report of the surgical specimen described the following findings: a uterine cavity covered by decidualized endometrium; presence of focally adherent villi with abundant necrotic decidua associated with hematic extravasation and covered by a trophoblastic double layer; and focal polarized endometrial hyperplasia with atypia and moderate amount of intervillous fibrin (Figures 4, 5 and 6). These findings were compatible with the diagnosis of partial molar pregnancy.
Source: Image obtained during the study.
Figure 4 Hematoxylin & Eosin (H&E) staining (10x). Hydropic degeneration of villi, showing inclusion of trophoblastic proliferation in the stroma.
Source: Image obtained during the study.
Figure 5 CD34 (10x). Hydropic degeneration of villi, showing focal overgrowth of the syncytiotrophoblast with abnormal proliferation of the vessels in the villi.
DISCUSSION
The placenta is an organ that develops during the first weeks of pregnancy and undergoes changes in its structure and function as the pregnancy progresses. This organ provides oxygen and nutrients to the fetus. In turn, placental villi are transport units that deliver oxygen and nutrients to the fetus (ensuring its development) and through which waste products are eliminated 4. Abnormal placentation is considered an underlying cause of various pregnancy complications such as miscarriage, preeclampsia, intrauterine growth restriction, and GTD. The latter comprises a heterogeneous group of diseases that occur due to abnormal trophoblast proliferation caused by inadequate fertilization. Furthermore, the pathogenesis of GTD is unique in that maternal lesions arise from fetal tissue rather than maternal tissue 5.
Within the diseases that comprise GTD, two major groups can be distinguished: gestational trophoblastic neoplasia and molar pregnancy. The latter group, in turn, includes two conditions, namely, partial hydatidiform mole and complete hydatidiform mole, which can be differentiated by their clinical presentation, macroscopic morphology and histology, and the patient's karyotype.
Molar pregnancy is considered the non-invasive form of GTD. Although it is usually benign, it is a precancerous disease that can become malignant due to chromosomal abnormalities that allow the formation of choriocarcinomas, which are tumors with invasive potential. In general, this malignant transformation is triggered by the activation of oncogenes, the inactivation of tumor suppressor genes, and the alteration of telomerase regulation 6.
The most common risk factors for hydatidiform mole are a history of molar pregnancy and extreme maternal age (both early and advanced) 7. However, other possible risk factors such as parity, history of abortion and maternal blood type have been proposed, although their association with the development of this disease has not been clearly demonstrated.
Typical clinical signs and symptoms of hydatidiform mole include abdominal pain, metrorrhagia during the first trimester of pregnancy, and a larger than expected uterine size for gestational age. Vaginal bleeding is caused by the separation of the chorionic villi from the underlying decidua, while pelvic and abdominal pain is due to the increased size of the uterus and increased myometrial contractility caused by blood extravasation 7. Other symptoms specific to this disease, although less frequent and mostly derived from elevated ßhCG levels, include hyperemesis, anemia, hyperthyroidism, respiratory distress, and early-onset preeclampsia (before 20 weeks of gestation). In addition, although rare, expulsion of hydropic vesicles from the vagina is also a pathognomonic sign of this disease 8.
In the case of clinical suspicion of GTD, the first diagnostic imaging test to be performed following an exhaustive gynecologic examination is a transvaginal ultrasound, since it allows assessing the size of the uterus, the presence or absence of an embryo, the pelvic extension of the disease, and placental vascularization, the latter by means of a Doppler ultrasound. In this regard, theca lutein cysts on transvaginal ultrasound may be identified in almost half of patients with complete hydatidiform mole, while the cystic appearance of the placenta or a deformed gestational sac may be initial ultrasound signs of GTD. Similarly, although the classic "snowstorm" sign is more common in cases of complete hydatidiform mole, it may not be seen on first-trimester ultrasound evaluation 3.
Once the transvaginal ultrasound has been performed, the following laboratory tests should be taken: complete blood count, Rh screening test, coagulation factor tests, quantitative hCG blood test, liver profile, renal function tests, and thyroid function tests. While determining total hCG levels rather than ßhCG levels is preferable, this option is not possible in all laboratories where such tests are processed, as was the case reported here. At this point, it should be noted that elevated hCG levels are often the first evidence of a possible molar pregnancy and that levels >100 000 mlU/mL suggest complete hydatidiform mole 7, but, as in the case presented here, there may be exceptions.
Maternal death from molar pregnancies is rare due to the early detection of the condition, protocolized care for its severity, and exhaustive surveillance of patients following surgical evacuation of the uterus 9. A chest X-ray before surgery is also required in order to rule out lung damage, as the findings of this radiological test are the basis for the staging of molar pregnancies proposed by the International Federation of Gynecology and Obstetrics (FIGO) 9. Further more, in cases of clinical suspicion of pulmonary embolism of trophoblastic origin, arterial blood gas analysis and computed axial tomography (CT) of the chest should be performed 7.
On the other hand, in cases of molar pregnancy, additional diagnostic imaging studies such as CT or magnetic resonance imaging (MRI) are not required if there is no evidence of vaginal metastasis on physical examination, no abnormal findings in chest X-ray, the results of liver function tests are normal, and there are no clinical symptoms and signs suggesting damage to other organs 9. If the patient's initial evaluation reveals metastatic cancer, an enhanced CT scan of the chest, abdomen, and pelvis, as well as a brain and pelvic MRI, should be performed; these studies should also be performed in patients with a histologically confirmed diagnosis of choriocarcinoma because of its high metastatic potential. The diagnosis of hydatidiform mole can only be confirmed by histological analysis of the evacuated uterine contents or the surgical specimen in case of surgical resection of the uterus by hysterectomy 7,9.
Despite the importance of early diagnosis of hydatidiform mole, other more frequent etiologies such as intrauterine pregnancy, ectopic pregnancy or early miscarriage should be considered initially in patients with metrorrhagia during the first trimester. Likewise, in cases in which a molar pregnancy is ruled out, extremely high ßhCG levels may be explained by twin pregnancy. Physical examination, together with ultrasound examination and measurement of hCG levels, will allow making a correct diagnosis 8.
In the case reported here, tumor formation, vaginal bleeding, and uterine size corresponding to a 20-week pregnancy could have been caused by other conditions such as uterine fibroids. However, the elevated ßhCG levels, positive pregnancy test and transvaginal ultrasound findings provided substantial evidence to reach the correct diagnosis.
Proper GTD staging, in this case hydatidiform mole, is critical for classifying patients and thus establishing specific treatments and adequate follow-up protocols 1. In this regard, in 2000, FIGO proposed an anatomic staging system with four stages (I to IV) to define the anatomical extent of the disease 10, which only takes into account the presence and location of metastases, without considering other risk factors. According to this classification, GTD in the present case would be classified as stage I because the disease is confined to the uterus.
Later, in 2015, the World Health Organization proposed a risk classification to determine the probability of response to treatment with single-agent chemotherapy. This new classification considers 8 items (age, history of pregnancy, time from gestational onset to disease onset, hCG levels, tumor volume, site of metastases, number of metastases, and previous chemotherapy) and in each one a score of 0, 1, 2, or 4 can be obtained. In this sense, a score <6 means that there is a low risk and a higher likelihood of response to treatment with single-agent chemotherapy, especially in patients with a score <4 7.
The treatment of hydatidiform mole should be adapted to the needs of each patient, with ultrasound-guided aspiration curettage being the preferred method; medical methods for uterine evacuation are not advised. Furthermore, the patient should be re-evaluated seven days after the procedure to determine the need for a second curettage if there is persistent vaginal bleeding or the presence of intra-cavitary debris 8. In perimenopausal women who report that they have already fulfilled their desire to be mothers (as in the case reported here) or who do not wish to preserve their fertility because, due to their age, they have a higher risk of gestational trophoblastic neoplasia, hysterectomy is an acceptable therapeutic option 1. Although ovarian preservation is recommended, even in the presence of theca lutein cysts, their removal eliminates the risk of local invasion; however, it is important to note that the risk of distant metastasis remains despite such removal 11.
On this matter, a recent meta-analysis supports the idea that hysterectomy could be the treatment of choice for hydatidiform mole in patients over 40 years of age who report having fulfilled their desire to be mothers 12; nevertheless, it is important to keep in mind that the uterus should be extracted without morcellation and that postoperative follow-up should be the same as that of patients undergoing evacuation of the uterus (serial monitoring of hCG levels) because they may still develop a gestational trophoblastic neoplasm requiring systemic treatment. Similarly, it is important to remember that Rh-negative patients should be administered anti-D immunoglobulin after uterine evacuation 13.
Adjuvant treatment with chemotherapy should be considered when hCG level are maintained or elevated after evacuation of the uterus or are >20 000 IU/L at 4 weeks after surgery; when there is histopathological evidence of gestational trophoblastic neoplasia; when there is evidence of metastatic disease; and in cases of vaginal, intraperitoneal or heavy gastrointestinal bleeding 7. None of these scenarios occurred in the case reported here, so adjuvant chemotherapy was not initiated.
With respect to the genetic study of the disease, as mentioned above, complete hydatidiform mole is usually diploid (46 XX/46XY), with all chromosomes of paternal origin. It results from fertilization of an enucleated egg by two sperm or by a haploid sperm that is then duplicated, resulting in a diploid (46XX/XY) androgenetic karyotype of paternal origin with absence of mitochondria. Rarely, complete hydatidiform moles are biparental and such cases are associated with an autosomal recessive condition predisposing to molar pregnancy 5. In contrast, in partial hydatidiform mole, a haploid egg is duplicated and fertilized by normal sperm, or a haploid egg is fertilized by two sperm, resulting in the expression of maternal and paternal DNA with a triploid karyotype (69, XXY; XXX; XYYY) 6.
The main histologic feature of GTD is a marked proliferation of villous trophoblast, together with hydropic degeneration of the chorionic villi. In complete hydatidiform mole, these villi are diffuse and surrounded by atypical trophoblast, whereas in partial hydatidiform mole, the villi usually have a normal appearance with focal hydropic changes and less trophoblastic hyperplasia and less atypia; moreover, in the former there is usually no fetal tissue 3.
GTD usually has a good prognosis, although its malignant potential lies in its capacity to invade the uterus and produce metastases. In this sense, detecting it in its early stages is critical since a delayed diagnosis may worsen its prognosis by reducing the success rate of treatment 3.
One of the strengths of this case report is that it was possible to follow and complete the diagnostic and treatment algorithm, including histologic confirmation of the disease by pathologic study of the resected surgical specimen. However, its main limitation is the lack of a genetic study, which could not be performed since an intraoperative sample was not collected for such analysis.
CONCLUSIONS
Although hydatidiform mole is a rare disease, it should be suspected in patients with metrorrhagia and symptoms of pregnancy. The initial signs and symptoms of this condition are neither alarming nor extraordinary but based on a good diagnostic algorithm and the information obtained during the anamnesis, physical examination and complementary tests, it can be included in the differential diagnosis of first-trimester metrorrhagia. This diagnosis can only be confirmed by histological analysis after evacuation of the uterus, and ultrasound-guided aspiration curettage is the evacuation procedure of choice. Early diagnosis of hydatidiform mole is of utmost importance as it allows timely treatment, thus improving its prognosis.