Introduction
Annually, in the United States, approximately 150 million intravascular devices are used for multiple purposes, mainly including the administration of fluids, medications and blood products; hemodynamic monitoring and renal replacement therapies.1End-stage chronic kidney disease, with a growing prevalence worldwide, and the need for hemodialysis as a treatment thereof constitute the main indication for the insertion of central venous catheters.2This is an important risk factor for the development of infectious complications, given that it negatively impacts the quality of life of patients and increases mortality rates up to threefold, when compared with the hospital population.3
The infectious or pathological commitment of the bloodstream, in this context, is considered as one of the main reasons for hospital admission, prolonged stay and adverse outcomes in users of these devices.4
Global initiatives for the study of the outcomes in patients on dialysis consider the presence of catheter-related infections as a potentially devastating complication, being the most common cause of morbidity and the second of mortality. The risk of sepsis attributable to this condition is one hundred-fold greater than that of the general population. In the same way, it is considered that hemodialysis catheters represent the greatest risk of bacteremia, sepsis and death compared with other vascular accesses.5
Magnitude of the problem
In Colombia, in 2013, the main device-associated infections were: symptomatic catheter-associated urinary tract infection, with 16.1% of cases; catheter-related bloodstream infection, with 13.7% of cases; and ventilator-associated pneumonia, with 3.3%.6.7 In other countries, the scene is no different: in North American databases 80,000 cases of intravascular catheter-related bloodstream infections are documented each year.1Latin America reports 12.5 cases of bacteremia for every 1,000 days of catheter use; the cost of Healthcare-Associated Infections (HAIs) is estimated between 28 and 33 billion dollars a year.1
All vascular access modalities involve a risk of complications. It is estimated a 32-fold increase in the risk of infection with temporary non-tunneled catheters, when compared with arteriovenous fistulas, and a 19-fold increase with the use of tunneled catheters.1The rate of catheter-related bacteremia (CRB) in non-tunneled central venous catheters (CVCs) ranges from 3.8 to 6.6 episodes/1,000 days of use of CVC and between 1.6 and 5.5 episodes/1,000 days of use of tunneled CVC. The use of a tunneled CVC implies a 7-fold to 20-fold increase in the risk of bacteremia with respect to the use of arteriovenous fistulas.8
Annually, approximately 30% of users of these devices experience a bacteremic or septic episode, despite the proven prophylactic strategies and the widely distributed guidelines on the prevention of access-related infections.9 Infection is the most common cause of morbidity and the second cause of mortality after cardiovascular disease in this population. 10
This analysis is intended to estimate the prevalence of infections associated with intravascular hemodialysis devices at the San Rafael Clinical University Hospital over a period of two consecutive years, 2015 and 2016. It also seeks to describe the local microbiological profile, evaluate the infectious complications that occurred (septic thrombosis, osteomyelitis, need for admission to the ICU, septic embolism and endocarditis), the outcomes in the population with infection, such as prolonged hospital stay, readmissions and death, and establish associations between sociodemographic factors, the presence of comorbidities, and catheter-related infection.
Methodology
A cross-sectional study of association, based on the review of medical records of patients hospitalized with a hemodialysis catheter at the San Rafael Clinical University Hospital (HUCSR) during the period between 2015 and 2016. The presence of hemodialysis catheter-related infection was evaluated according to criteria taken from the Protocol of Surveillance of Device-Related Infections in Public Health, National Institute of Health, 2015,7 in order to make a description of the clinical findings, type of infection, local microbiological profile, treatment received by the patients and outcomes. The study population consisted of patients older than 18 years, treated in the emergency and hospitalization (general and ICU) services, of whom a convenience sample was taken and all patients treated in the institution were included. The cases were selected according to the established inclusion criteria; patients with a blood culture report of less than 100,000 CFU, negative blood cultures and initiation of antibiotic therapy prior the collection of cultures of the catheter tip were excluded. To estimate the minimum size of the statistical sample, the following assumptions were assumed: an estimated proportion of catheter-associated bloodstream infections of 13.7%,2 an acceptance error of 10% and a confidence level of 95%, assuming a binomial distribution, for a total of 64 subjects.
The clinical and demographic variables of the patients were collected only by the research team, in order to maintain the confidentiality of the data. The information was obtained from the clinical history and data reports of the institutional infection committee and was recorded, stored and organized in a database in Excel format designed for that purpose.
The present study had the endorsement of the institutional ethics and research committee, before the data collection. It is considered a study without risk according to Resolution 8430/93 of the national regulations.11
Results
Between 2015 and 2016, a total of 320 hemodialysis patients were treated in the institution. Of them, 18 had intravascular device-related infection, and for this reason the prevalence of the period of hemodialysis intravascular device-related infection in the University Hospital was 5.62 %. The average age in the group with infection (Group 1) was 55.3 years, with a standard deviation of 16.5 years, while in the group without infection (Group 2) it was of 60.27, with a deviation of 16.9 years. 66.67 % of Group 1 consisted of men; while in group 2, 60.93 % were men. In Group 1, 100% of patients came from the city of Bogotá. Of the patients with hemodialysis device-associated infection, 26.82% was constituted by diabetics vs. 38.8% without such diagnosis (Table 1).
Table 1 Demographic characteristics of the population under study in the San Rafael Clinical University Hospital between 2015 and 2016
| DAI* n (%) | No DAI n (%) | |||
| Variables | Characteristics | 18 (5.6) | 302 (94.3) | |
| Average | 55,3 DE 16,5 | 60,27 DE 16,9 | ||
| Age | Minimum | 23 | 16 | |
| Maximum | 84 | 90 | ||
| Gender | Female | 6(33,3) | 118 (39) | |
| Male | 12 (66,6) | 184 (60,9) | ||
| Bogotá | 18(100) | 281 (93) | ||
| Casanare | 0 (0) | 1 (0,3) | ||
| Provenance | Cundinamarca | 0 (0) | 1 (0,3) | |
| Boyacá | 0 (0) | 1 (0,3) | ||
| No data | 0 (0) | 17 (5,6) | ||
| Diabetics | Yes | 7 (38,8) | 81(26,82) | |
| No | 11 (61,1) | 221(73,1) | ||
The most used catheter insertion site was the right jugular in 33.33% of patients, followed by the right femoral in 27.78% and the left jugular in 16.67%. The time of placement of the catheters ranged between two weeks and one month, 44 % (Table 1). About 45% had previous infection due to the catheter and about 44% used antibiotics prior to the episode; likewise, in the clinical manifestations at admission, 16.67% had secretion in the wound (tunnelitis).Control blood cultures were performed in 77.78% of the cases, of which 77% became negative. The rest of infected patients (22.2%) did not have control cultures (Table 2).
Table 2 Clinical characteristics associated with the intravascular device and antecedents related thereto at the San Rafael Clinical University Hospital between 2015 and 2016
| DAI* n (%) | No DAI n (%) | ||
| Variables | Characteristics | N=18 (5,6) | N=302 (94,3) |
| Right femoral | 5(27,7) | 57 (18,8) | |
| Left femoral | 0 (0) | 24 (7,9) | |
| Tunneled | 4 (22,2) | 47 (15,5) | |
| Type of catheter | Right jugular | 3(16,6) | 69 (22,8) |
| Left jugular | 6(33,3) | 24 (7,9) | |
| AV fistula | 0 (0) | 59 (19,5) | |
| No data | 0 (0) | 22 (7,2) | |
| Less than two weeks | 3(16,6) | 79 (26,1) | |
| Between 2 weeks and one month | 8 (44,4) | 46 (15,2) | |
| Time with the catheter | Between 1 month and 6 months | 0 (0) | 2 (0,6) |
| More than 6 months | 7 (38,8) | 48 (15,8) | |
| N/A | 0 (0) | 127 (42,0) | |
| Previous DAI episode | Yes | 8 (44,4) | 5 (1,6) |
| No | 10 (55,5) | 297 (98,3) | |
Regarding the use of initial antimicrobial treatment, the most commonly used empiric antibiotic was vancomycin plus piperacillin tazobactam in 55.56% (n = 10). After the report of the blood cultures, 88.89% of the patients required a change of antibiotic, which was oxacillin in 44.44% of cases.
Patients with a diagnosis of hemodialysis catheter-associated infection had an average stay of 17 days. 38.8% of patients of the same group were transferred to the intensive care unit (ICU). Of them, 22.2% required invasive mechanical ventilation and 27% required vasopressor support during their hospital stay. 5.5% were readmitted due to complications and 22.2% died. Studies such as echocardiogram and Doppler of blood vessels were performed to 100% of infected patients in order to determine associated complications. Endocarditis was found in 16.6 %, septic thrombosis in 27.7 %, septic embolism in 11.1 %, and osteomyelitis was diagnosed in 5.5 % of cases (Figure 1).
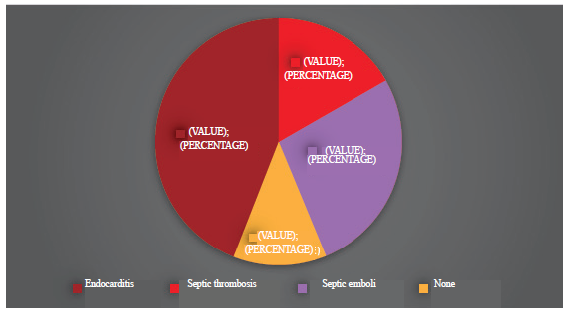
Figure 1 Classification and Regression Tree (CART). Incident patients (0) green and prevailing patients (1) orange.
In relation to the Charlson scale, which estimates the survival probability, a statistically significant correlation (p = 0.004) was found in the values: 4.13 vs. 3.73 in the prevalent event, with respect to the non-infected group, according to what was expected in terms of impact on mortality.
Associations with different variables and with the hemodialysis devices-associated infection (DAI) were made, and the following results were obtained:
Among those patients who had a diagnosis of diabetes (38.89%), a statistically significant association with the development of device-associated infection was not evidenced with OR 1.73, 95% CI (0.65-4.63) (p = 0.26), but it was more frequent. Likewise, a statistically significant association between the device-associated infection and the risk of death was not found (22.22% vs. 19.87%, respectively), with OR 1.15, 95% CI (0.36 - 3.62) p = 0.80, although it was higher in the infection group, probably because of the sample size. The hemodialysis catheter-associated bacteremia increased the risk of developing complications such as septic thrombosis, with an OR 11.50. 95 % CI 12.5-1056 (p = 0.00), as well as the need for admission to the intensive care unit, with an OR of 4.16, 95 % CI (1.52-11.37) (p = 0.00).
Discussion
The need to use high flow intravascular devices to perform dialytic therapies in patients with renal insufficiency implies an increase in the exponential risk for the development of bloodstream infections and negatively impacts the clinical condition and the environment of the patient. The higher number of days of hospital stay, the risk of complications (septic thrombosis, endocarditis, and need for admission to ICU, among others) and the relationship with higher mortality rates in this group of patients make important the knowledge in the preventive, diagnostic and therapeutic approach to this condition.
The present study compares local data with regional statistics and world literature on the subject. It was found a lower prevalence with respect to the results of other works in centers of similar complexity, 5.62 vs. 6.7 cases per 100 patients/month in the United Kingdom.4
As it has been reported by other authors,8 this study indicates that the rates of infections and other events were substantially higher in patients who underwent dialysis with the use of catheters, especially non-tunneled. The high rates of catheter-associated infections are a concern, since both the number of patients undergoing hemodialysis and the percentage of patients with dialysis catheters increase every year.12,13
In the results of the present study, the most frequently isolated germ was methicillin-susceptible Staphylococcus aureus, with a frequency of 61.1%, followed in order of frequency by enteric gram-negative bacilli. According to databases from the United States, gram-positive cocci are the bacterial flora most frequently isolated in relation to endovascular devices. Coagulase negative Staphylococcus can be found in up to 45% of cases; Staphylococcus aureus, in between 22% and 29% of cases; enterococci in 9% and, as another important group, gram-negative bacilli are isolated in up to 30%2(Table 3).
Table 3 Relationship of the local microbiological profile and resistance profiles of blood cultures according to their results in the population with DAIat the San Rafael Clinical University Hospital between 2015 and 2016
| Isolated Microbiological Strains | n (%) =18 |
| MRSA* | 1 (5,5) |
| MSSA** | 11 (61,1) |
| Klebsiella spp | 4 (22,2) |
| Pseudomonas aeruginosa | 1 (5,5) |
| Other | 1 (5,5) |
* MRSA: Methicillin-resistant Staphylococcus aureus **MSSA: Methicillin-susceptible Staphylococcus aureus
It is highlighted that this study is the first in a population with these characteristics, in the San Rafael Clinical University Hospital, so that it sets a precedent for future work. We emphasize that the prevalence in the institution is lower compared to that evidenced in other centers. Despite the small sample size, there are statistically significant associations between the admission to the ICU, the presence of septic thrombosis and this disease.
The sample size did not allow to establish a significant relationship between infection and mortality derived from it, although it was higher in the infected group. Endocarditis (16.67%), septic thrombosis (27.78%), septic embolism (11.11%) and osteomyelitis (5.56%) were the complications presented. Among the most relevant results, it was found a statistically significant association between septic thrombosis and the need for admission to the ICU (p = 0.0000).This type of complications has an important morbidity and a non-negligible mortality. Likewise, they constitute the most frequent cause of removal of the device.14 However, a statistical relationship between the noted complications has not been previously established in the literature reviewed.15
We consider valuable the lower number of hemodialysis catheter-associated infections with respect to other centers of similar complexity. It reflects the adequate implementation of preventive measures, as well as the correct techniques of insertion and care of the devices. Finally, analytical studies are required to evaluate the behavior of the disease over time.
Conclusions
The prevalence found in the period of analysis, regarding intravascular hemodialysis devices-associated infection at the San Rafael Clinical University Hospital, was 5.62%, comparatively lower than that of other centers of similar complexity. All patients came from the city of Bogotá, the main population attended in the institution. The ages ranged between 16 and 90 years. The male gender prevailed in the infected group.
The initial antimicrobial scheme was the conjugation of piperacillin tazobactam + vancomycin, although it was required to decrease the spectrum in most cases, according to the microbiological isolates. The germ most frequently found as the causative agent was methicillin-susceptible Staphylococcus aureus, in agreement with the world literature, followed by the group of enteric gram-negative bacilli.
A statistically significant relationship was found between DAI and complications such as endocarditis, 27.78% septic thrombosis, 11.11% septic embolism and 5.56% osteomyelitis, as well as an increased risk of admission to the intensive care unit, need for mechanical ventilation and vasopressor medications. (Table 4).
Table 4 Prevalence ratio of the different outcomes in patients with and without catheter-related infections at the San Rafael Clinical University Hospital between 2015 and 2016
| Variable | DAI (n=18) | 95 CI | No DAI (n=302) | 95 CI | p |
| Septic thrombosis | 27,78 | (16,6 - 33,3) | 0,33 | (0,1 - 1,64) | 0,0000 |
| Admission to ICU | 38,89 | (27,7 - 49,9) | 13,25 | (9,8 - 21,59) | 0,0008 |
| Diabetes mellitus | 38,89 | (27,7 - 49,9) | 26,82 | (25,43 -38,6) | 0,399 |
| Death | 22,22 | (16,6-27,7) | 19,87 | (17,6 - 27,98) | 0,951 |
| Readmission | 5,56 | (2,26 - 7,60) | 0,00 | (0,00 - 1,54) | 0,053 |
| Osteomyelitis | 5,56 | (2,26 - 7,60) | 0,00 | (0,00 - 2,01) | 0,053 |
| Septic embolism | 11,11 | (5,54 - 22,22) | 0,00 | (0,00 - 3,42) | 0,000 |
| Endocarditis | 16,67 | (11,11 - 29,89) | 0,00 | (0,00 - 1,58) | 0,000 |
The average length of stay was 17 days, approximately twice compared with other causes of admission.
The mortality in patients with DAI was 22.2% in the period evaluated, without establishing a statistically significant relationship with the event, given the sample size.
Ethical responsibilities
Protection of people and animals
The authors declare that no experiments were performed on human beings or animals for this research.
Data confidentiality
The authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consent
The authors state that patient data do not appear in this article.
Contribution of the authors
Preliminary project, project, data collection and analysis: Rafael Fernando Pino, Internal Medicine Resident; Leonardo Arturo Pimienta, Internal
Medicine Resident; Javier Alberto Gómez, Internal Medicine Resident.
Thematic and methodological tutor: Dr. Maite Hurtado Uriarte, Nephrologist.
Methodological and statistical tutor: Dr. Mariana Villaveces, Epidemiologist.











 texto en
texto en 


