Introduction
The proportion of older people in the general population is steadily increasing worldwide, with the most rapid growth in low- and middle-income countries (1). This demographic change is the consequence of socioeconomic development and better life expectancy. However, population aging also has important implications for society - in diverse areas including health systems, labor markets, public policy, social programs and family. A successful response to the aging population will require capitalizing on the opportunities that this transition offers, as well as effectively addressing its challenges (2).
In Argentina 10.2% of the population consists of people older than 65 years. The older population is estimated to be19.3% in 2050 and 24.7% in 2100, based on data of The World Bank (3).
Older adults have socio-biological features, characteristic diseases and special needs, which carry important concerns and require specific attention (4). Longevity entails an increase in the occurrence of acute clinical conditions, and the prevalence of chronic ones (5). However, it should be taken into account that there are at least two types of aging: the usual one, which appears when aging-related changes reduce the homeostatic capability of the organism, and the successful aging which is unusual, and appears when aging related-changes are slightly marked, leading to insignificant functional changes compared to young individuals (6).
Kidneys are affected by the aging process, which results in many effects on the renal system. As we have mentioned, older population is heterogeneous - some have a progressive decline in their glomerular filtration rate (GFR) of around 1 ml/year as of 30 years of age, whereas in healthier adults the decline in GFR is much more subtle. Lindeman et al. reported the results of longitudinal studies showing that the rate of decline in renal function was 0.75 ml/min/year. However, as many as 1 out of 3 subjects showed a stable GFR over time (7).
Fliser et al. proposed that GFR changes linked to aging might be the consequence of an altered responsiveness to vasodilators and vasoconstrictors (8,9). This theory is based on observations that the filtration fraction increases with aging, due to a disproportionate fall in renal plasma flow relative to GFR. Other authors have attributed the age-related GFR reduction to the aging-induced glomerulosclerosis process and/or the reduced metabolic rate characteristically found in older individuals (10). However, it should be considered that a preserved GFR in an older individual could be secondary to successful aging, or the stage I (GFR: ≥90 ml/min/.73 m²) of chronic kidney disease (CKD) in an older individual. The presence of CKD markers (proteinuria, altered renal ultrasound, etc.) and/or hyperfiltration inducing comorbidities can contribute to distinguishing these alternative settings.
This phenomenon of the preserved GFR in older people has not been thoroughly studied, even less in the Southern Cone. The aim of this study was to estimate the prevalence of preserved GFR, and to explore the association between cardiovascular risk factors and preserved GFR in older individuals.
Methods
Study design and setting
This cross-sectional study collected data on baseline CKD markers from the ongoing CESCAS study (9). The CESCAS study is a population-based prospective cohort study, which entails a probabilistic sample of 7524 non institutionalized mainly urban men and women between 35 and 74 years of age, representing the general adult population of four cities in Argentina, Chile and Uruguay. Details on the design of the study were published elsewhere (11). For the purpose of this study, we focused on 1571 older adults (65-74 years old) with a valid creatinine measurement.
Participants and recruitment
As the prevalence of cardiovascular disease (CVD) risk factors was considered likely to vary by age, gender and geographical area, the study sampling was stratified by these variables, following a complex sampling design that consisted of four stratified stages to obtain a representative sample of the following cities: Marcos Paz (Argentina), San Carlos de Bariloche (Argentina), Temuco (Chile) and Canelones Department (Uruguay). Participants who accepted to be part of this study were interviewed at home and invited to visit a local facility for clinical examination and laboratory measurements.
Data collection
The protocol for the CESCAS I Cohort Study has already been published (11).
Trained interviewers gathered information about participant characteristics including demographic, socioeconomic and healthcare insurance, personal and family history of cardiovascular diseases and risk factors such as high blood pressure, dyslipidemia and diabetes mellitus, as well as current pharmacological treatment.
Trained personnel measured height and weight from all participants during the clinic visit. Each measurement was taken three times, and the average of the three values was used for analyses. In addition, three systolic (SBP) and diastolic (DBP) blood pressure measurements were obtained using standardized procedures.
Laboratory measurements
After an overnight fast, venous blood was collected for plasma glucose, serum lipid profile and creatinine. Serum creatinine was measured by the modified kinetic Jaffé method (IDMS-TRACEABLE). LDL cholesterol levels were calculated using the Friedewald equation for participants with triglyceride levels <400 mg/dl.
Study variables
The estimated GFR (eGFR) was defined using the CKD-Epidemiology (CKD-EPI) collaboration equation using serum creatinine as a filtration marker based on the latest Kidney Disease Improving Global Outcomes (KDIGO) guideline (12).
As the GFR normally decrease with aging, we defined preserved GFR using eGFR (CKD-EPI) > 80 ml/min/1.73 m2 based on the metanalysis of Pottel et al 2017 (13).
Diabetes mellitus was defined as fasting plasma glucose ≥126 mg/dL or self-reported physician diagnosis or use of anti-diabetic medication) (14). Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg, diastolic blood pressure (DBP) of ≥90 mmHg or being on anti-hypertensive therapy at the time of enrollment (13,14). Obesity was defined through the BMI index ≥30 and dyslipidemia was defined by total serum cholesterol ≥240 mg/dL and/or LDL cholesterol ≥160 mg/dL and/or HDL cholesterol <40 mg/dL and/or triglycerides ≥200 mg/dL and/or current use of medication to lower serum lipids (16).
Within behavioral risk factors, we considered low intake of fruits and vegetables as <5 servings per day, which was estimated using a self-administered food frequency questionnaire validated in Argentina, Chile, and Uruguay (17). Physical activity was measured using the International Physical Activity Questionnaire (IPAQ), and low-physical activity was defined as 600 MET-minutes/week of total physical activity using the metabolic equivalent (MET) formula (18). History of cardiovascular disease was self-reported, including any of the following conditions diagnosed by a physician: acute myocardial infarction, angina, heart failure, cerebrovascular events, peripheral vascular disease or coronary or peripheral revascularization. History of cancer was self-reported as diagnosed by a physician (11,19,20).
Pharmacological treatment with drugs that affect the renal function was defined using the Anatomical Therapeutic Chemical (ATC) code in the following drug groups: angiotensin-converting enzyme inhibitors (ACEI), non-steroidal anti-inflammatory drugs (NSAIDs) and proton pump inhibitors (PPIs).
12-Item Short Form Health Survey (SF-12) measures of physical status was used as a frailty indicator (MCS12) (21). SF-12 component scores were calculated as standardized scores towards the USA population as a reference group. This reference population has a mean score of 50 with a standard deviation (SD) of 10.
Healthy older adults
We defined healthy older adults when one or more of the following conditions were absent: hypertension, diabetes mellitus, and obesity or cardiovascular disease (acute myocardial infarction, angina, heart failure, cerebrovascular events, peripheral vascular disease, coronary or peripheral revascularization) (22).
Statistical Analysis
Weighted percentages for categorical variables and weighted means for continuous variables along with 95% confidence intervals (CI) were used to describe the characteristics of the study population and the prevalence of eGFR >80 ml/min/1.73 m2. For prevalence of healthy older adults, number of participants without cardio metabolic conditions or cardiovascular disease over the total number of participants. Prevalence Ratio (PR) was calculated using the following formula: PR= OR / (1+ p in non-exposed * (OR-1)) and Adjusted Attributable Prevalence Fraction was calculated as (p in non-exposed × (PR − 1)) / (p in non-exposed × (PR − 1) + 1). Backward stepwise logistic regression analysis was used to study the effect of cardiovascular risk factors on eGFR >90 ml/min. A p-value <0.20 was required for retention of each variable in the final model. Results are presented as adjusted odds ratio (aOR) and 95% CI. All statistical analyses were performed using the statistical software Stata IC, version 14.2 (Stata Corp., College Station, TX, USA). Due to the complex sampling design, we used the svyset command to account for sample stratification and weighting to provide unbiased estimates of the population parameters. Statistical significance was defined as a two-sided p-value <0.05 for all tests.
Results
Of the total sample of 1571 adults aged 65-74 with complete laboratory data on plasma creatinine, the median eGFR was 85.5 ml/min/1.73 m² (IQR: 73.1-91.3). 962 subjects had an eGFR >80 ml/min/1.73 m2. Of those, 154 were healthy older adults (Weighted Prevalence= 17.0 %).
Regarding the targeted healthy older population, the mean of SBP was 22.9 mmHg points lower, DBP 8.2 mmHg points lower, glycemia 20 mg% points lower and BMI was 4.7 points lower than in non-healthy older adults. All these variables were significantly lower in relation to the features of these parameters in the non-healthy older people. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) use was also lower in the healthy older group. Conversely, quality of life in the physical score was higher, 3 points higher in the healthy group with no difference in the mental domain. See table 1.
The prevalence of healthier older adults with eGFR >80 ml/min/1.73 m2 was higher among men (19.0 vs. 15.6), in current smokers: 29.8 and lower in subjects with dyslipidemia (p= 0.02). See table 2.
The multivariable logistic regression model showed that presence of dyslipidemia aOR 0.6 (0.4; 0.9), current smoking aOR 1.9 (1.2; 2.9) and quality of life in physical domain aOR 1.03 (1.0; 1.1) were independent factors associated with an eGFR >80 ml/min/1.73 m2. Based on the formula for the adjusted attributable fraction for prevalence, this represents 8% due to dyslipidemia, 9% to smoking and 1% to physical QoL. See table 3.
Discussion
In the present study, the prevalence of preserved GFR (≥80 ml/min/1.73 m²) in healthy older individuals (age ≥ 65 years) from the general population of the Southern Cone of Latin America was 17%. This older population presented similar prevalence of cardiovascular risk factors as mentioned in others population-based studies in the region (11,23,24).
The reduction of eGFR secondary to aging was originally reported by Davies et al. in 1950, when they measured eGFR by using insulin clearance, finding a decrease from 122.8 ± 16.4 ml/min/1.73 m² at 30 years of age to 65.3 ± 20.4 ml/min/1.73 m² at 90 years of age in 70 healthy individuals.(25) This finding was later reconfirmed by Rowe et al in 1976, using 24 hours creatinine clearance in a cross-sectional analysis where 548 subjects showed a statistical difference in creatinine clearance at age 30 to 80 (26). However, aging-related eGFR reduction has a lower declining rate (0.75-1 ml/min/year) than the one usually induced by CKD (≥3 ml/min/year). Lindeman et al. obtained serial creatinine clearances from 254 normal volunteers followed between 1958 and 1981 in the Baltimore Longitudinal Study of Aging. Even though they documented a mean decrease in creatinine clearance of 0.75 ml/min/year, they also observed that one third of all subjects being followed had no absolute decrease in renal function with age (7). However, “preserved eGFR “could be attributed not only to a successful renal aging but also to a hyperfiltration status induced by an early stage of CKD (stage I) (6,27). In addition, the presence of the main prevalent conditions, most of them CKD inducers, such as hypertension, diabetes mellitus, dyslipidemia, and their pharmacological treatment have been used as proxy markers to distinguish healthy older individuals from unhealthy ones in our study.
Tabla 1 Description of main characteristics of healthy and unhealthy older adults with eGFR ≥80 ml/min
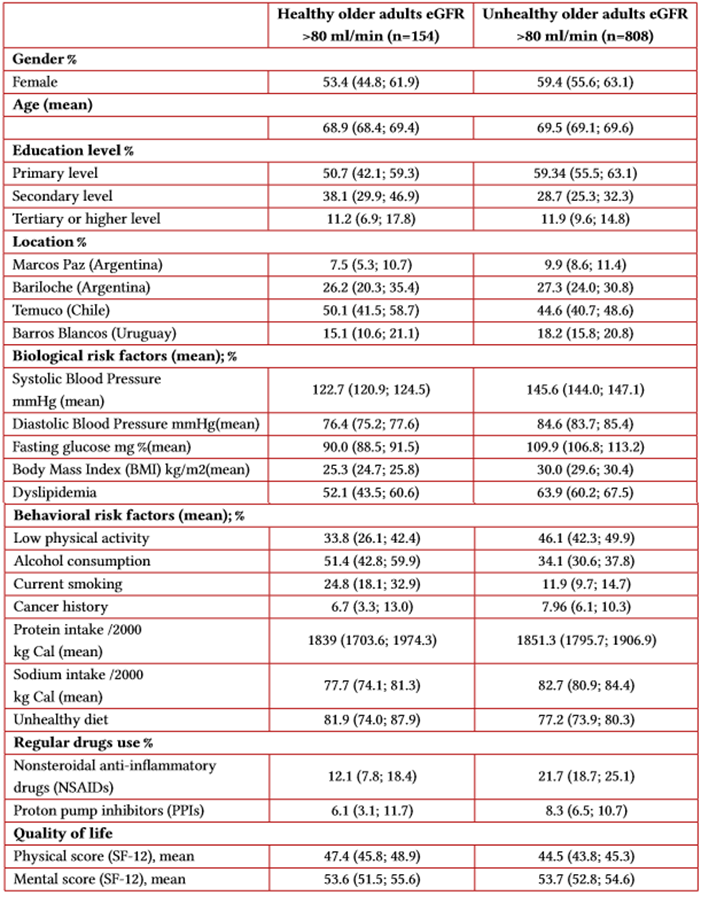
Source: own elaboration.
Tabla 2 Prevalence of eGFR ≥ 80 ml/min/1.73m2 healthy older adults among different variables sub groups
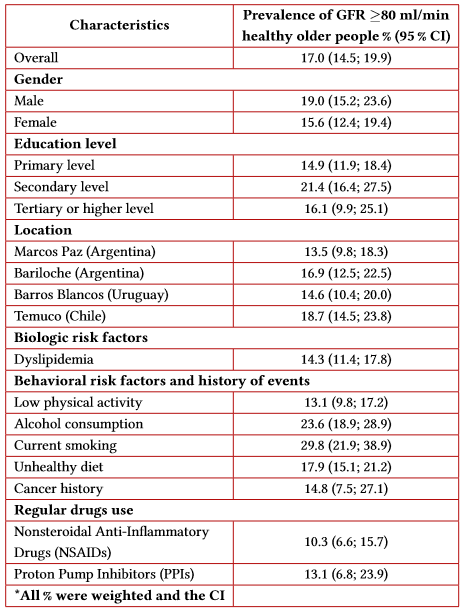
Source: own elaboration.
An eGFR >80 ml/min/1.72 m² was more prevalent in men, smokers, and those individuals who had lower serum lipid levels, and higher physical score. Regarding the relationship between male sex and preserved eGFR in healthy older people, it is difficult to be explained since it is already known that renal diseases are more prevalent in men than in women, and testosterone has been postulated as one of the substances involved in promoting age-related glomerular sclerosis (26-28). However, it is already known that the female hormonal protective factor is lost in older individuals (30). Moreover, previous studies performed in successful renal aging populations reported no univocal associations between gender and preserved GFR, since they fluctuated between the presence of some gender preponderance (13,31) until no gender preponderance (32-34). Obviously, there are other unknown underlying factors which are unknown and may determine this phenomenon (11,29,30,35).
Tabla 3 Logistic regression model and adjusted attributable prevalence fraction (%) for the association between cardiovascular risk factors and eGFR ≥ 80 ml/min/1.73m2 in older adults
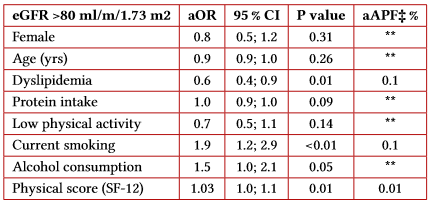
Source: own elaboration.
As to the finding of a higher prevalence of eGFR > 80 ml/min/1.73 m² in smokers who had lower serum lipid levels and higher physical scores, it could be speculated that these are characteristics of a group of robust and very active older individuals who require neither diet changes nor lifestyle restrictions (28,29). In this sense, there is attributed to evidence that physical activity could be beneficial both to prevent GFR decline and to improve the quality of life in these patients (35).
It is worth pointing out that it is well-known that the aging process has an asynchronous nature, and that successful aging of one organ (e.g. a kidney with a preserved GFR value) can coexist with the pathologic aging of another organ (e.g. a brain affected by dementia) (6). It has been estimated that genes play a role in about 25% of the variation in longevity, whilst environment and individual variability may have an even higher impact. A progressive defect in DNA repair mechanisms, accompanied by a shortening of the telomeres is a characteristic of normal physiological aging (35). Older individuals who have no hyperfiltration inducing disease should be carefully evaluated in future studies in order to better understand their renal physiology, as well as the underlying mechanisms.It should be mentioned that unlike CKD-related eGFR reduction, age-related eGFR (usual aging) presents no altered urinalysis, serum creatinine, urea, hemoglobin, or parathyroid hormone levels, or abnormal renal ultrasound. Since this was a retrospective analysis of the data obtained from the CESCAS study, these clinical markers could not be measured in our study. However, the main prevalent conditions, most of them CKD inducers, such as hypertension, diabetes mellitus, dyslipidemia, and pharmacological treatment were used as proxy markers to classify healthy older individual from unhealthy ones.
Conclusion
The present cohort study documented that 17% of healthy older individuals have preserved glomerular filtration rate (eGFR ≥ 80 ml/min/1.73 m2) despite their advanced age. This phenomenon of successful renal aging deserves further investigation to find out what the implicated mechanisms would be.















