Introduction
Due to their working conditions, teachers have a high risk of feeling high stress levels, voice symptoms, and low sleep quality. Previous studies reported that voice problems [1-6], poor quality of sleep [7,8], and high levels of stress [9-11] are health conditions often reported by teachers due to their occupational demands and sometimes “negative” work environment. Voice symptoms have been reported to have a significant impact on physical, psychological, occupational, and social aspects of teachers’ life [12]. Sleep quality has been reported as one important factor for maintaining good physical and mental health [13]. A previous publication reported that the prevalence of low sleep quality among teachers was high, with more than 60% of teachers having “bad sleep”, and stress was associated with low sleep quality [14]. In addition, stress has been reported as a psychosocial condition that may affect teachers’ health [11], with a prevalence ranging between 34% and 69% [9,15].
A comparable situation is reported among college professors. Atará-Piraquive [16] estimated that 35% of Colombian college professors reported voice problems. Lemos reported that 21% of participating professors presented high levels of stress associated to their perception of high ambiguity, high number of occupational tasks to perform, homeworking conditions, family-work unbalanced relationship, among others [17]. Sanabria-Mazo reported that 49% of the participants had low sleep patterns [18]. In addition, Carrillo-González found that self-reported intermediate and elevated levels of sleep quality were associated with statistically significant higher standard deviation of sound pressure level in connected speech, and may be associated with a low probability of self-reported voice complaints [19]. Therefore, teachers with these three health conditions may represent important economic costs for them, for the educational institutions, and for the society in general [20].
Although the prevalence of these three conditions is elevated among teachers, few studies have investigated the productivity costs associated to them. The estimated cost represented in lost workdays and treatment of voice disorders among teachers in the United States was around $2.5 billion annually [21]. Cantor-Cutiva and Burdorf indicated that 97% of work-related voice disorders’ costs were indirect costs for voice-related absenteeism and productivity loss at work [22]. They found that indirect costs of a teacher with voice symptoms were around US$492 per month and their productivity loss due to voice symptoms was around 36% of the average teacher’s monthly wage [22]. In addition, Lages et al. reported that occurrence of work-related absences for voice disorders ranged between 3% and 63% [23]. Likewise, some health conditions were associated with reduced work ability among teachers such as not sleeping well at night [24]. These empirical findings suggest that employees who sleep less than 6 hours per day were, on average, about 2.4% less productive due their absenteeism or presenteeism than those sleeping between 7-9 hours per day [25]. In the United Kingdom, teachers absenteeism due to mental health problems raised from 213.000 days in 2004 to approximately 312.000 days in 2017, which represents a financial cost of over 65 million pounds [26].
Although previous studies have reported the impact of voice disorders, high stress levels, and low sleep quality on teachers’ performance and quality of life, there is a lack of studies on the economic impact of these three conditions. Moreover, it is unknown how homeworking and online classes due to COVID-19 pandemic affect these costs. For this reason, the purpose of this cross-sectional study was to estimate the productivity costs associated with self-reported voice symptoms, low sleep quality and high stress levels among college professors during homeworking in times of COVID-19 pandemic.
Methods
Study design and participants
Colombian college professors participated in this cross-sectional study. Data collection took place between September and December 2021. Professors were invited to participate via email, and registrations were performed through a registration form in Google Suite. Inclusion criteria was defined as follows: 1) participants should be active college professors who worked in the institution, and 2) participants should have previously feel either voice symptoms, low sleep quality or high stress levels. One exclusion criterion was defined as working most of the time in a different university. The institutional Medical Ethics Committee reviewed and approved this study.
Data collection procedures
After registering to participate in this study, professors received a Zoom link via email for the data-collection meeting (according with their availability), a Google link to the Work-related health and working conditions Questionnaire, the assigned ID (alphanumeric code to guarantee confidentiality and privacy of the data), and the informed consent form. The informed consent form and the questionnaire were sent before the meeting to allow participants to review and identify possible questions. Then, during the meeting, the researcher (second author) instructed the participants on how to send via email the signed informed consent form, answered questions to the participant (if any), and asked the participant to fill in the questionnaire.
Work-related health and working conditions Questionnaire
This questionnaire included previously standardized questions on sociodemographic, lifestyle habits, working conditions, voice functioning, and validated items such as the Voice-Related Quality of Life (VRQOL), Vocal Fatigue Index (VFI), stress quality item, and sleep quality item [16,22,27-32]. The first part of the questionnaire contained questions on sociodemographic information (age, gender, marital status). The second part of the questionnaire included questions on occupational daily voice use, days per week of voice use, years of experience, students per class, lifestyle habits, and health conditions. In the third part, we included the Spanish versions of the Vocal Fatigue Index [29] and the Voice Related Quality of Life [30]. The fourth part included questions on health-care use, voice-related absenteeism, and productivity loss due to voice symptoms based on Cantor-Cutiva and Burdorf [22], Elo’s question about stress levels [31] and Sonnentag’s question about sleep quality [32]. The stress item was: “Stress means a situation in which a person feels tense, restless, nervous, or anxious, or is unable to sleep at night because his/her mind is troubled all the time. Do you feel this kind of stress currently?” (Spanish version: El estrés es definido como una situación en la cual una persona se siente tensa, inquieta, nerviosa, ansiosa o es incapaz de dormir en la noche porque su mente está preocupada todo el tiempo. ¿Siente este tipo de estrés actualmente?). The response was recorded on a Likert scale, in which 1 means not at all and 5 mean very much (as in the original version) [31]. The question for sleep was: “How do you evaluate your last night's sleep?” (Spanish version: ¿Cómo evaluaría el sueño de su noche anterior?). The response was also recorded on a Likert scale, with 1 meaning very poor and 5 meaning very good (as in the original version) [32].
For this study, we focused on the questions about stress levels, sleep quality, voice symptoms, and reduction in productivity due to these three health conditions.
Independent variables
Three independent variables were defined: stress levels, sleep quality and voice symptoms. For voice symptoms, we used the single question: “Have you had voice symptoms in the past month?” (Spanish version: ¿Ha tenido síntomas de voz en el último mes?). The response was recorded on a dichotomous scale (yes/no) [22]. However, participants were instructed that voice symptoms may include the presence of vocal fatigue, hoarseness, dysphonia, sore throat, among others.
Costs associated to productivity reduction due to voice symptoms, high stress levels, and low sleep quality
Participants were asked to indicate how much their voice symptoms, high stress levels or low sleep quality interfered with their productivity at work in a 10-point scale in which 0 means no interference and 10 mean complete interference [22,33]. In addition, they were asked to inform the number of days that they worked with less productivity due to voice symptoms, high stress levels or low sleep quality. Also, we asked participants about their average monthly salary.
Data analysis
All statistical analyses were performed by means of SPSS 25 (IBM Corporation). Descriptive statistics were used for characteristics of the study population. Proportion (in percentage) of participants with low sleep quality, high stress levels, and voice symptoms was calculated. We determined the costs of reduction in productivity multiplying the number of days worked with less productivity with the fraction of productivity loss because of voice symptoms, high stress levels or low sleep quality per teacher by the wage per day.
Data distribution for productivity reduction costs associated to the three health conditions were assessed by means of the Shapiro-Wilk test (Z=0.764 - p-value=0.00 for productivity reduction due to voice symptoms; Z=0.860 - p-value=0.09 for productivity reduction due to high stress levels; Z=0.823 - p-value=0.00 for sleep; Z=0.897 - p-value=0.00 for stress). The results indicated that data were not normally distributed (except for productivity reduction due to high stress levels). We did not assess data distribution either for the variable “voice symptoms”, because it was a dichotomous variable or productivity reduction due to low sleep quality as the data set was small and it was not possible to run the test.
Results
Participant characteristics
In total, fifty-eight college professors participated in this study. During data collection, twenty-nine subjects did not inform their average monthly salary. Therefore, they were included in the analysis of productivity reduction but excluded in the costs analysis. Among the fifty-eight participants, 35 were females and 23 were men. Men professors were older, had more experience as teachers, and worked more daily hours using their voices compared with female professors. The days of teaching per week and number of students per class were higher for female participants compared with male participants (Table 1).
Table 1 Characteristics of fifty-eight participating professors per gender
| Variable | Females (n=35) | Males (n=23) | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age | 45.9 | 8.7 | 52.1 | 13.1 |
| Experience teaching (years) | 14.4 | 8.2 | 21.5 | 12.0 |
| Hours of teaching per day | 5.8 | 2.0 | 5.9 | 2.0 |
| Days of teaching per week | 4.9 | 1.2 | 4.6 | 1.1 |
| Number of students per class | 29.9 | 12.4 | 24.3 | 10.1 |
Voice symptoms, low sleep quality, and high stress levels
Among all participants, 19% of them reported having had voice symptoms in the last month. Only two male subjects reported low sleep quality (3%). Female professors reported higher levels of stress (14%) than their male pairs (10%) as shown in Table 2.
Productivity reductions due to voice symptoms, low sleep quality, and high stress levels
On average, there was a greater interference at work among male professors (2.8) compared with females (2.0) due to voice symptoms. Likewise, males showed more productivity loss due to stress levels (6.3) compared with their female colleagues (5.1). Male professors showed a 1.5 reduction in productivity due to sleep problems, whereas female participants reported a longer duration of voice symptoms (4.5 days) and high stress (14 days) compared to males (2 and 5.7 days respectively). Male professors with low sleep quality reported an average duration of 2.5 days (Table 3).
Table 3 Average scores of productivity loss associated with low sleep quality, stress, and voice symptoms per gender
| Females (n=35) | Males (n=23) | |||
|---|---|---|---|---|
| Scores of productivity interference | Media | SD | Media | SD |
| Voice symptoms | 2.0 | 2.2 | 2.8 | 2.5 |
| Sleep problems | 0.0 | 0.0 | 1.5 | 0.7 |
| High stress levels | 5.1 | 2.2 | 6.3 | 2.0 |
| Days of productivity loss | Days | SD | Days | SD |
| Voice symptoms | 4.5 | 5.6 | 2.0 | 2.0 |
| Sleep problems | 0.0 | 0.0 | 2.5 | 2.1 |
| High levels stress | 14.0 | 10.0 | 12.7 | 9.5 |
Costs associated to productivity reduction due to voice symptoms, high stress levels, and low sleep quality
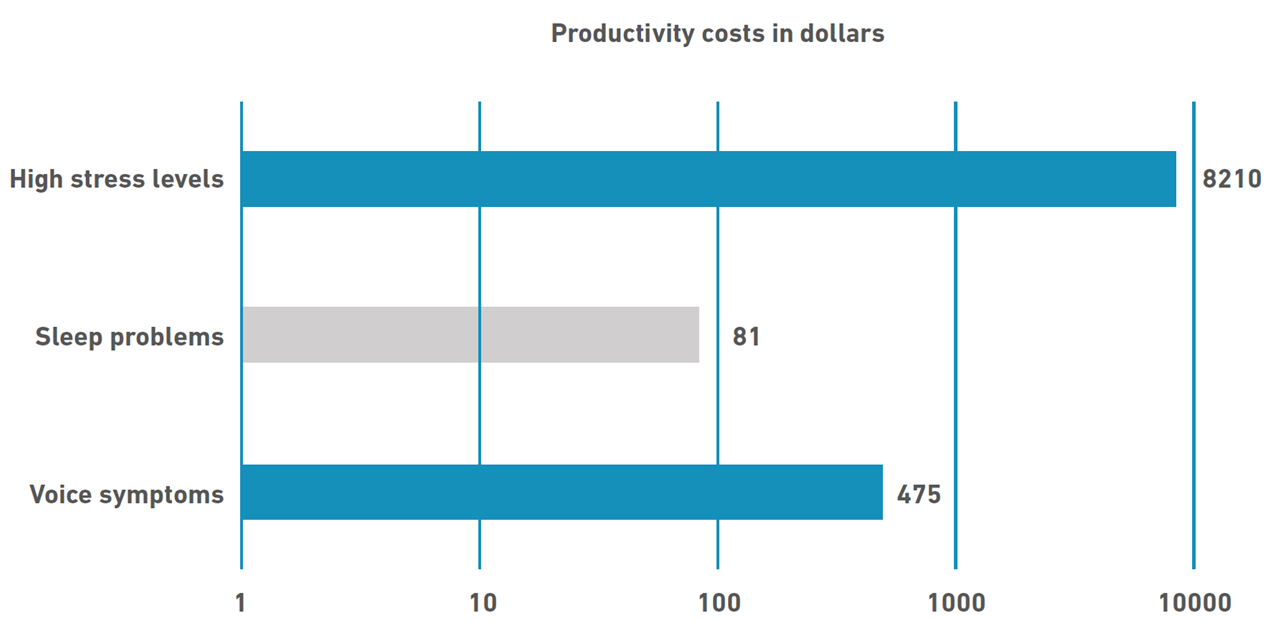
As previously mentioned, 29 out of the 58 participants were included for costs analysis. As shown in Figure 1, average productivity reduction costs associated to low sleep quality represented COP$319.733 (US$81). College professors who reported high stress levels had average productivity reduction costs of COP$32.345.925 ($8,210), whereas average productivity reduction costs due to voice symptoms were COP$1.872.703 (US$475).
Discussion
In this study, we calculated the productivity reduction associated with low sleep quality, high stress levels, and voice symptoms among fifty-eight college professors from a Colombian public university. We found three important results: 1) College professors showed higher report of high stress levels (24%) compared with voice symptoms last month (19%) and low sleep quality (3.4%); 2) Stress represented most of the productivity reductions among participating professors, followed by voice symptoms and low sleep quality; and 3) Productivity costs associated with high stress levels were higher (COP$32.345.925) compared with voice symptoms (COP$1.872.703), and low sleep quality (COP$319.733).
Concerning our first result, college professors showed higher report of high stress levels (24%) compared with voice symptoms (19%) and low sleep quality (3.4%). This result agrees with Kyriakou et al., who informed that 25% of college professors reported stress frequently [34]. However, our result on stress prevalence disagrees with other studies among college professors that reported that 67% of their participants had tension and stress [35] associated with their teaching organization process [36]. Regarding voice symptoms, other studies have reported prevalence between 35% [16,34] and 45% [37], which is higher that the prevalence found in this study. Our results on the prevalence of low sleep quality is in agreement with a previous study that reported a prevalence of 3% among their participants [38]. One possible explanation for these disagreement between our results and previous studies is the homeworking (and quarantine) conditions that have changed the ways that teachers work and live. A second explanation is the instruments used to determine voice symptoms, self-reported stress, and self-reported sleep quality. Since COVID-19 pandemic caused that several countries went into strict quarantines (including Colombia), we were not able to meet in-person with the participants but just online, which may have influenced the results. Future studies are needed to confirm these hypotheses.
Regarding our second result, stress was the health condition with the highest productivity reduction duration (13 days). There is little information available from other studies on the duration of high stress levels and low sleep quality among college professors. However, it has been reported that workers who report dissatisfaction with their life in general or experience high stress levels, felt less productive at work when performing jobs requiring communication, cognitive and interpersonal skills [39]. In the same direction, disturbed sleep may be an effective predictor of future long-term absences due to poor health. Low sleep affects work performance, and work-related issues can hamper sleep, creating a downward spiral in both personal well-being and work success [40]. Concerning voice symptoms, Cantor-Cutiva and Burdorf reported that schoolteachers with voice symptoms have had these symptoms for 5 days or less, which is slightly higher than our results (3 days) [22].
About the third finding, productivity reduction costs associated with high stress levels were higher (US$8,210) compared with low sleep quality and voice symptoms. Burton et al. reported that productivity costs among corporation workers with high stress levels were estimated between US$1,392 and US$2,592 per employee [39]. These results are lower than our results, which may be explained by the impact of having a “service” occupation (occupation where the action are receive by people instead of objects) compared with “desk work” in other companies. Previous studies have reported that “service occupations” (i.e., health workers or teachers) have higher stress levels compared to other occupations because students/patients/relatives increase the job pressure and stress. Concerning our results on voice symptoms, productivity reduction costs in this study were around US$475, which agrees with previous studies among college teachers (around US$492) [22]. This means that although voice disorders are widely researched among teachers, their impact remains; therefore, activities and programs to reduce the prevalence of voice disorders and their consequences are still needed. Lastly, low sleep quality’s productivity reduction costs were COP$319.733 ((US$81), whereas previous research reported costs of around US$1,967 per worker annually [41]. As we mentioned previously, no research had investigated the productivity costs of sleep problems among teachers; consequently, our results were not compared with a teacher’s population, which may explain the disagreement between our results and Rosekind’s results.
Conclusion
Our results show that college professors are occupational voice users with a high risk of feeling high stress levels. Previous studies have reported that stress is a prevalent and costly problem in today’s workplaces [42]. Consequently, the presence of elevated stress levels reported among the participants could be a consequence of the changes in working conditions due to homeworking in times of COVID-19 pandemic.
From our results, it can also be concluded that management stress strategies should be included when designing workplace based health programs in educational settings, because these strategies may help to reduce the occurrence of this health condition and the productivity costs associated with stress [43,44].
On the other hand, early interventions are recommended because productivity reduction costs due to high stress levels, low sleep quality or voice symptoms can increase if these conditions become either more severe or chronic, causing limitation in activity [45].
In conclusion, productivity reduction costs were higher for professors who reported high levels of stress, followed by participants with self-reported voice symptoms and low sleep quality, which highlight the importance of prioritizing activities to reduce stress levels and voice symptoms in workplace health promotion programs implemented in educational settings.