Introduction
Esophageal high-resolution manometry (HRM) can be defined as a system that measures pressures of the entire pharyngoesophageal segment using a nasogastric catheter equipped with several sensors capable of identifying small pressure gradient changes with great anatomical precision.
The first manometry system dates back to the 1940s and is currently known as conventional manometry. It was a system that used unidirectional water flow through a catheter to verify intraluminal pressure in an indirect way through resistance to water flow. High-resolution manometry (HRM) emerged as a natural improvement over conventional manometry, previously scarcely used for proximal pharyngoesophageal region studies, due to the imprecise data obtained by using very sparse capture sensors and the slow response of water-perfused systems [1].
The HRM that we currently use has a catheter with over 24 sensors arranged usually every 1 cm. Each of these sensors may be arranged radially. Although there are HRM water-perfused systems, most are solid-state with highly responsive sensors able to detect variations of up to 6,000 mmHg/s with an accuracy of 1 mmHg along the entire pharyngoesophageal segment. Thus, HRM provides simultaneous objective data regarding the pharynx, upper esophageal sphincter (UES), body of the esophagus, lower esophageal sphincter (LES), and proximal stomach [2].
HRM provides a real-time temporal-spatial graph with colors corresponding to the pressure intensity, which is easy to understand and analyze. In this graph, the closer to blue, the smaller the pressure gradient, and the closer to dark red, the greater the pressure gradient in the region of interest. It is worth mentioning that in this graph it is possible to identify exactly to which anatomical region the colors correspond to (see Figure 1) [3].
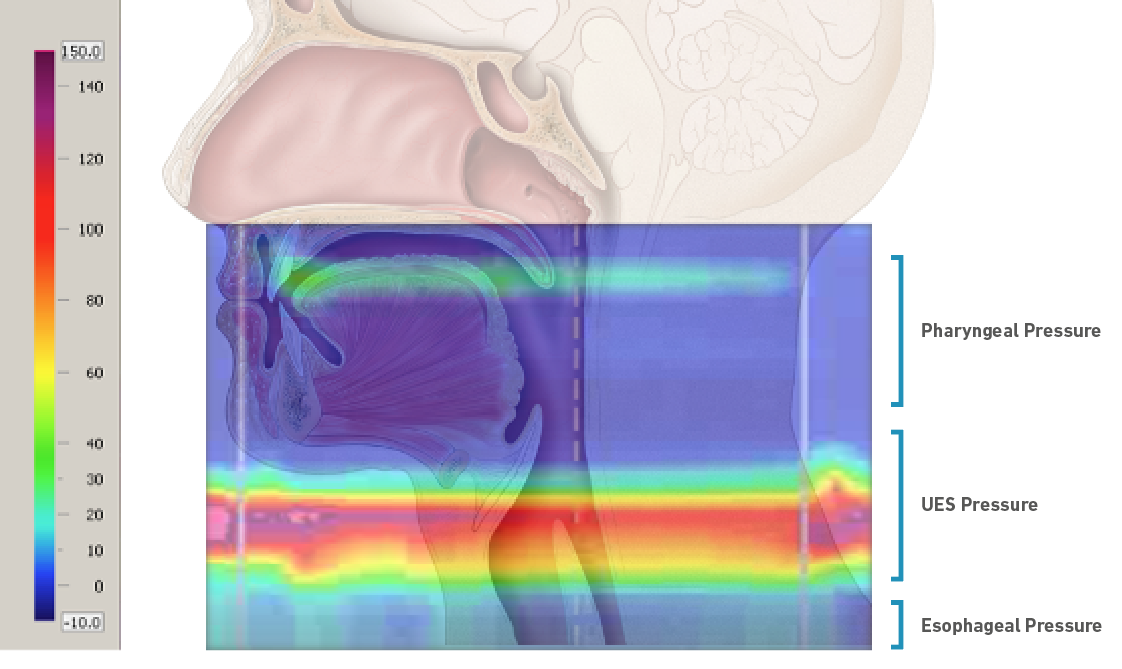
Figure 1. High-resolution manometry spatiotemporal plot demonstrating pharynx, upper esophageal sphincter, and esophagus pressures during the emission of a sustained vowel /æ/ superimposed on a sagittal section of the human head and neck. On the left, the color scale is related to pressure intensity. On the right, the anatomical regions with phonation responses.
HRM usage for investigations and dynamic evaluation of the pharynx, esophagus, and the entire swallowing process provided researchers and clinicians with unprecedented physiological information impossible to obtain by other methods, such as videofluoroscopy, endoscopy, ultrasound or electromyography [4]. HRM has been demonstrated to be extremely useful in distinguishing between normal and altered swallowing, calling the attention of speech therapists working with dysphagia patients [5-7].
Based on such a huge established validity for clinical and scientific usage with dysphagia researchers, HRM started to draw the attention of voice scientists as well, since the pharyngoesophageal segment includes structures involved in phonation, such as the pharynx and velopharynx [8]. In addition, phonation provokes pressure responses in the UES and esophagus, which represent important structures for the understanding and study of vocal physiology, as we will see below [9,10].
Throughout this manuscript, we will explore the main contributions, technological improvement, and the reasoning that has stimulated this technology usage to improve phonation physiology knowledge.
Reflections
Voice and esophagus connections
Esophageal pressure measurements began to attract vocal scientists’ attention in 1952, when Fry and his collaborators unlocked a new perspective for breath studies, concluding that intra-esophageal pressure could provide an estimate of intrathoracic pressure [11].
From this perspective, researchers started investigating esophageal pressures as a possible way of estimating both pulmonary and tracheal pressures, the latter of particular interest to the voice area, because it would bring advances in terms of subglottic pressure, which corresponds to the expiratory air pressure retained below the glottis with the approximation of the vocal folds and represents the main mechanism used to regulate vocal intensity during speak and singing voice [12-14].
The first studies that tested the possibility of obtaining subglottic pressure from esophageal measurements used a balloon inserted through the nose and positioned at the esophagus as well as a needle inserted in the tracheal region to measure subglottic pressure. The two methods were performed concurrently so that both pressure measurements could be compared. Studies concluded that intraesophageal pressure measurements provide a valid estimate of subglottic pressure during phonation, except at the end of prolonged phonation [14,15].
Due to the procedure discomfort and invasiveness, this same technique was performed only in a few other voice studies. Those were able to clarify that subglottic pressure is not exactly equal to esophageal pressure because subglottal pressure depends on lung volume and elasticity, which do not reflect at the esophagus. However, sudden changes in esophageal pressure are directly associated with changes in subglottic pressure with almost identical magnitudes. In addition, esophageal pressures are low at high lung volumes, when the expiratory lung elastic force is high, and increase with decreasing lung volume, as the lung elastic force decreases [15-19].
Esophageal balloon usage, despite being extremely useful for these first researches and conclusions, has some limitations such as the lack of control and precision over its positioning inside the esophagus besides the restricted data provided corresponding only with the area that surrounds it. These limitations were overcome with the advent of HRM, a modern system capable of evaluating the contractility of the entire pharyngoesophageal segment, providing objective, dynamic and standardized measurements that facilitates the interpretation of data and, therefore, the applicability with diverse objectives in different areas of knowledge [20-22].
The increasing number of studies and publications encouraged researchers from different areas such as pneumology, otorhinolaryngology, and speech therapy to initiate using this technology in the study not only of pressures, but also of physiological events involving laryngeal framework movement since the UES is mainly composed of the cricopharyngeal muscle that attaches bilaterally to the inferior lateral margin of the cricoid plate and, therefore, moves together with the larynx [23].
Owing to all the possible contributions of HRM to the voice area, some studies began to be conducted with a small number of participants so that the various hypotheses could be tested. Most of the studies were carried out by multidisciplinary teams involving gastroenterologists, otorhinolaryngologists, and speech therapists, making it clear that the more we can change the perspective, the better our understanding about the physiology of phonation will be.
High-Resolution Manometry and Phonation Events
The first publication that clearly shows a phonatory event in a high-resolution topographic manometry plot occurred in a study that aimed to demonstrate the establishment of normal swallowing pressure values along the velopharynx and UES. In order to easily identify the velopharynx during the examination, the researchers asked the participants to vocalize the plosive consonant “ka” several times (Figure 2). From the images generated by the manometry software, researchers were also able to perceive that the pressures in the pharyngeal region were greater when swallowing than when vocalizing [24].
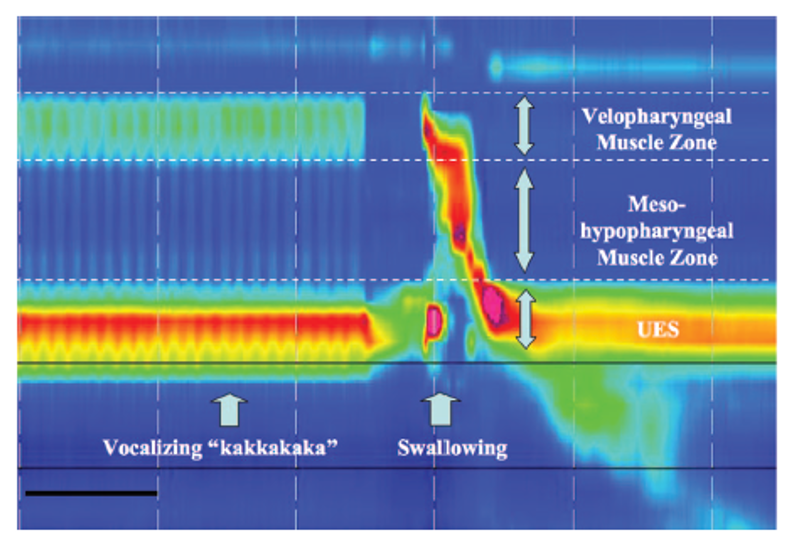
Figure 2. High-resolution manometry spatiotemporal plot during “kakakakaka” vocalization followed by swallowing (24). Reprinted from Takasaki et al. (2008), with permission from John Wiley and Sons.
In the same year, a pioneering article about phonation using HRM data was published. The researchers used HRM plot to determine and characterize the effect of phonation on the intraluminal pressures of the upper gastrointestinal tract and test the hypothesis that during phonation the UES would exert a significantly greater pressure compared to the body of the esophagus and the LES protecting the larynx against reflux events. The results demonstrated that phonation actually increases the pressure gradient in the UES region in greater magnitudes than those found in the stomach and esophagus, suggesting the existence of a contractile reflex of the UES to phonation [9]. This 2008 publication appeared for a long time as the only parameter about manometric data and phonation. An increased pressure gradient at the UES region during phonation was confirmed in other studies that came a few years later.
Only in 2021, a new and more complete study sought to explore and understand pressure changes in the pharyngoesophageal segment during different phonatory stimuli. This group used HRM to investigate the pressures of singers in the thorax, UES, and pharynx regions during different phonatory tasks performed at low, moderate, and high intensities and compared them with pressures at rest. The study, in addition to illustrating the different pressure magnitudes for the researched regions at different intensities in a didactic way, also demonstrates that all absolute values are higher during vocalization than at rest. In addition, the increase in vocal intensity is accompanied by an increase in intraluminal pressure in the thorax (or body of the esophagus) and the UES, the latter always higher than those presented by other regions, displaying a more intense color at the topographic plot. The research also demonstrates that high-intensity vocalizations activate a larger area of the UES region, as shown in Figure 3 [10].
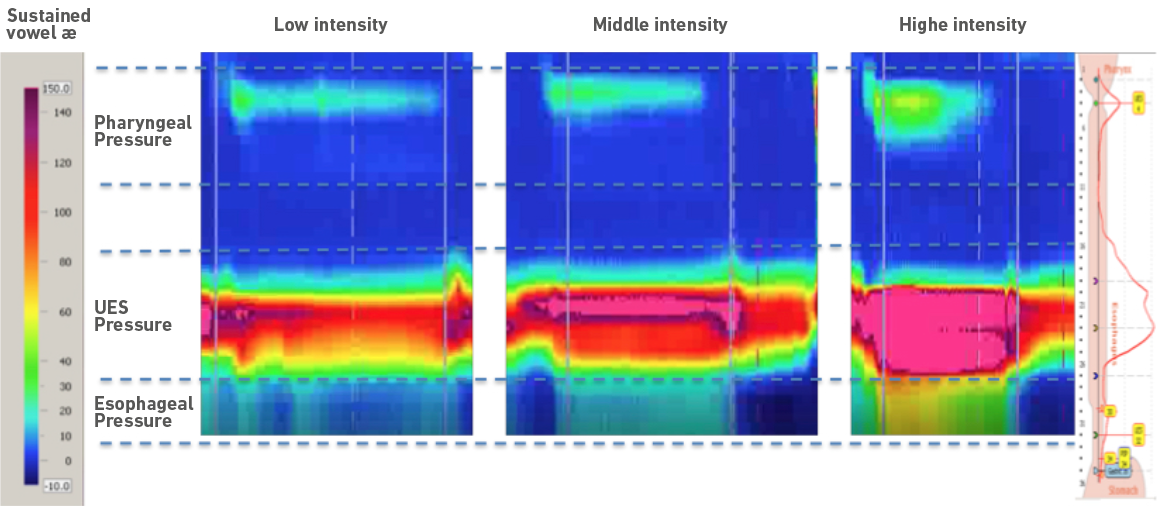
Figure 3. High-resolution manometry spatiotemporal plot during the vocalization of a sustained vowel /æ/ produced at low, medium, and high intensity demonstrating the pressure gradient in the pharynx, upper esophageal sphincter and esophagus regions.
The UES pressure gradient was studied not only in healthy voices, but also in disordered voices. Assuming that a UES dysfunction may represent a possible cause for dysphagia in patients with muscle tension dysphonia (MTD), Van Houtte and colleagues used HRM to compare UES pressures in people with and without MTD diagnosis. The authors found no statistical difference between the UES pressures when comparing both groups at rest. However, during phonation, the UES pressure threshold is higher in all phonatory tasks performed by the group with MTD. The authors concluded that patients with MTD possibly have a hyperfunction of the cricopharyngeal muscle [25].
The cricopharyngeal muscle is the target of several studies that seek to understand the normal physiology and the possible changes that occur during swallowing and may cause dysphagia [26,27]. Those data contributed with the voice area providing information about cricopharyngeal activation during volitional and non-volitional tasks. As demonstrated by HRM studies, UES pressures generated by cricopharyngeal muscle activation seem to be more associated with non-volitional tasks, as swallowing and exhaling, than with volitional tasks such as phonation. Voluntary tasks, such as phonation, may have greater cortical influence exhibiting more variability and independence between the UES and the cricopharyngeal muscle [28].
Apart from contributing to the understanding of pressures in the pharyngoesophageal segment during speech, HRM has also proved to be useful as a biofeedback tool for the larynx vertical excursion training. With the HRM catheter placed, ten professional singers were asked to raise and descend their larynges during a sustained vowel. Then, the screen with the topographic plot of the HRM was exhibited to the singers, instructing them about the position of the UES that would correspond to the larynx height. Visualizing the UES location at the screen, singers were then encouraged to, once again, raise and descend their larynx. As a result, all singers were able to improve their vertical larynx excursion with biofeedback, mainly when descending it [29].
Air pressure, one of the central themes for vocal production, also gains new perspectives with the use of HRM. This pressure, which is directly related to phonatory efficiency, is usually obtained by methods that limit the possibilities of natural vocalization because of lips occlusion besides providing a single point measure data [30]. As HRM uses a nasogastric catheter, the oral region remains free for speaking and singing, enabling the data collection to reflect the natural physiology of phonation. Understanding air pressures using HRM can bring new information about the flow throughout the entire vocal tract, since the probe has multiple sensors arranged longitudinally, offering simultaneous data in real time. The air pressures in the hypopharynx, oropharynx, and nasopharynx, impossible to obtain with conventional methods, can now be simultaneously measured during phonation and even during exercises proposed in the vocal clinic, such as the semi-occluded vocal tract exercises (SOVTE) [31].
The influence that SOVTE exerts on stress in the pharyngeal and UES regions during phonation was the object of a recent study, demonstrating that stress increases pressure in the UES region during vowel phonation, but not during SOVTE. These results help us to understand the existing mechanisms between voice and stress, which represents the cause of several voice disorders. In addition, those results strengthen engagement for more lines of research that uses HRM to provide advances about voice treatments [32].
As HRM is not yet a technology that takes part into voice and phoniatrics laboratories, many researchers carry out studies comparing data obtained with HRM to other sorts of exams and better-known procedures so that physiology can be understood from different perspectives [9,33].
Recently, a study compared data obtained by electromyography, sound, bioimpedance, and high-resolution manometry to differentiate swallowing from vocalization events. The topographic plot obtained with HRM clearly differentiates both events. In light of this, the authors concluded that the HRM topography represents an almost perfect precision tool to measure and detect swallowing events, confirming the ease of data interpretation using this technology [34].
HRM has enabled new perspectives for neuromotor research such as the understanding of the vagus nerve activation physiology, fundamental for phonation. When the recurrent laryngeal nerve (RLN) is functioning properly, the larynx can act as a sphincter, preventing aspiration occurrence and allowing phonation. The RLN and the pharyngeal plexus are also responsible for the UES closure, and this activation works as a laryngeal protection against laryngopharyngeal reflux events through the activation of the cricopharyngeal muscle [35].
The shared esophagus and glottis innervation relationship through vagus nerve stimulation was reviewed by means of HRM to test the hypothesis that a possible vagus nerve inefficiency would be behind cases of vocal folds hypomobility and abnormal esophageal function as those observed in cases of ineffective esophageal motility, suggesting a possible relationship between the two conditions. The results obtained are extremely interesting, exhibiting that UES inefficiency is significantly greater in patients with hypotonia of the superior laryngeal nerve or recurrent laryngeal nerve, further strengthening the idea that many answers we seek about laryngeal events can be answered by esophagus exploration [36].
HRM has already clearly brought contributions to the physiology of phonation with relatively easy data acquisition and interpretation. There is a growing number of publications in the last 2 years, but much more are required with larger samples allowing researchers to extract from HRM all it can bring to the voice science.
Some factors such as the high cost of the equipment and the need of a trained physician to perform the test may explain the small number of studies carried out so far. Nor can we rule out the fact that the test is invasive and, although tolerable, causes a little discomfort. Nevertheless, the studies are extremely feasible and necessary.
Conclusion
Due to the procedure discomfort and invasiveness, HRM represents not a clinical but a research investigative tool that has proven to be extremely useful in obtaining pressure measurements of the entire pharyngoesophageal segment during phonation, contributing with the comprehension of many voice aspects such as subglottic pressure, vertical laryngeal excursion, cricopharyngeal muscle activation, air flow, muscle tension associated with vocalization, and pressure variations associated with different phonatory stimuli.
The topographic plot generated by HRM software makes it possible to visualize physiological events that occur at the pharynx, UES and body of the esophagus during phonation in real time beyond indicating pressure intensity by color allowing easy data interpretation.
HRM enables aerodynamic pressure measurements with anatomical precision, physiological dynamism, and total phonatory and articulatory freedom. This unique data acquisition method can bring to the voice science much more reliable information about the speaking, singing, regular, and disordered voices, closing many gaps between science and practice.















