Introduction
The incidence of pituitary adenomas (PA) is 3.9-7.4 cases per 100,000 (Daly & Beckers, 2020) and some of the pathological entities they cause are considered rare diseases (Orphanet Report Series, 2021). They represent 10 % of all intracranial neoplasia and are usually benign (Blanco, Fernández & Escribano, 2016), although the benign-malignant paradigm in pituitary neuroendocrine tumors is being questioned (Tortosa, 2019). PA are classified according to their size into microadenomas (<1 cm) and macroadenomas (≥1 cm), and in functional (FPA) and nonfunctional (NFPA) depending on their hormonal activity (Blanco, Fernández & Escribano, 2016).
Both FPA and NFPA affect the health-related quality of life (HRQoL), even after the disease control when hypopituitarism is treated (González et al., 2016). Sexual and reproductive health (SRH) is an important dimension of the HRQoL, as it is an expression of the human integral health closely linked with individual welfare. The World Health Organization (WHO) considers reproductive health (RH) as a key aspect of sexual health (SH), defined as the state of physical, mental, and social well-being in relation to sexuality, and not merely the absence of infirmity, dysfunction, or discomfort (OMS, 2018). SRH is closely related to physical and mental health and is significantly influenced by sociocultural aspects (Omo-Aghoja, 2013).
One of its dimensions, the sexual function (SF), is a crucial part of the individual’s identity and it is relevant in all health and disease stages. It consists of the transition between phases from arousal to relaxation, with pleasure and satisfaction (APA, 2013). SF is related to sexual and gender roles, individual health status, and other biopsychosocial variables (Simon & Lukas, 2017).
PA can affect different aspects of the SRH such as hypopituitarism in acromegaly, oligomenorrhea and decreased sexual desire (DSD) in Cushing’s disease (CD), hypogonadism and DSD in PA-secreting prolactin (PRL), erectile disorder (ED) in men, subfertility, and infertility (Blanco, Fernández & Escribano, 2016; Krysiak et al., 2016). Hypopituitarism also occurs in many patients with NFPA (González et al., 2016). Treatments for PA, which combine surgery, radiotherapy, and/or pharmacotherapy, may likewise impair SRH (Blanco, Fernández & Escribano, 2016; González et al., 2016), and specifically, SF can be affected by hormonal disturbances, compressive effects, the comorbidities, the associated psychological disorders, and the changes produced in physical appearance (Balercia et al., 2007; Novoa et al., 2013; Tortosa, 2019). Nevertheless, SF in patients with PA is still little explored, considered as determined by medical factors, and insufficiently understood regarding its relationship with psychosocial parameters which have been suggested as SF determinants in people with chronic illnesses (Daleboudt et al., 2013).
To our knowledge scant studies have researched SF in patients with PA, comparing different groups of diagnosis (FPA/NFPA), sex (women/men), and age (young adults/middle-aged adults), and relating SF performance with psychosocial and health variables. The present study aimed to evaluate SF in patients with PA and to determine its relationship with some sociodemographic, health, SRH, and psycho-affective variables.
Materials and methods
The study was approved by the local ethics committee (Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán-INCMNSZ, with registration number CONBIOÉTICA-09-CEI-011- 20160627). The principles of the Declaration of Helsinki were followed, and informed consents were obtained from all patients.
A comparative cross-sectional study was carried out between September-November 2016, and from December 2018-August 2019. Seventy-three patients with PA (52 women and 21 men) between 20- 59 years old, diagnosed according to the 2017 WHO Classification (Osamura et al., 2017), were recruited from the Neuroendocrinology outpatient clinic of the Department of Endocrinology and Metabolism at INCMNSZ, Mexico City. They were selected in a non-probabilistic convenience way and distributed into two age groups: young adults (20-39 years old) and middle-aged adults (40-59 years old) (Kurubilla et al., 2018).
Seven patients were excluded because of hysterectomy (3 women), brain aneurysm clipping (1 man), Sheehan syndrome (1 woman), early-stage pregnancy (1 woman), and for not completing the evaluation (1 woman). To exclude patients with major cognitive disorders, they completed a brief cognitive assessment: the Mini-Mental State Exam during the first phase of the study and the Montreal Cognitive Assessment during the second phase, both validated for the Mexican population (Ostrosky-Solís, López-Arango & Ardila, 2000; Águila-Navarro et al., 2018). No patient was diagnosed with moderate or major cognitive disorder (Llamas-Velasco et al., 2015; Loureiro et al., 2018).
The participants were asked to complete a semi-structured interview aimed to collect sociodemographic, general health, and SRH information, some of which was supplemented with their medical records. All patients completed the Beck Anxiety Inventory (BAI) and the Beck Depression Inventory (BDI), validated for the Mexican population, to evaluate the presence and severity of anxiety and depression, respectively (Jurado et al., 1998; Robles et al, 2001). These multiple-choice self-reporting scales have a total score range from 0–63, a cut-off value to discriminate the presence of anxiety ≥6 in BAI (Robles et al, 2001) and depression ≥10 in BDI (Jurado et al., 1998), and specific ranges to describe their severity (Beck & Steer, 1987; 1990).
Women were subjected to the validated Spanish version of the Female Sexual Function Index (FSFI) (Blümel et al., 2004), which is a self-report questionnaire including 19 items subdivided into six domains of the SF performance for the last four weeks: sexual desire, sexual arousal, vaginal lubrication, orgasm, pain and sexual satisfaction (Rosen et al., 2000). For each domain, a score was calculated and the higher scores indicated better performances. The total SF score, being the sum of the six domain scores, may range from 2-36, with lower values indicating a higher symptom burden. Women with a total SF score of <26.55 were classified as presenting impaired SF (Wiegel, Meston & Rosen, 2005) and each sexual domain with a score <65 % (<3.9) was considered impaired (Barut et al., 2018).
Men were subjected to the validated Spanish version of the International Index of Erectile Function (IIEF) (López et al., 2013), which is a self-administered questionnaire including 15 items of the SF performance for the last four weeks, subdivided into five domains: erectile function (EF), orgasmic function, sexual desire, overall satisfaction, and intercourse satisfaction (Rosen et al., 1997). For each sexual domain, a score was calculated and the higher scores indicate better performances. The six domain scores were added to obtain the total SF that lies from 5-75, with higher scores indicating better SF. The total EF score ranged from 6-30 (Hernández et al., 2017), with a cut-off for ED <26 and the following intervals to describe its severity: no ED (26–30), mild (22–25), mild–moderate (17– 21), moderate (11–16), and severe (1–10) (Cappelleri et al., 1999). A cut-off value was used for the other sexual domains based on a qualitative analysis in which the diminished and/or the presence of difficulties was interpreted as an impairing indicator. Therefore, each domain under a 60 % score (<6 in orgasmic function, sexual desire, and overall satisfaction, and <9 in intercourse satisfaction) was considered as impaired. The cut-off value for the total SF score was determined by adding the cut-off values of each sexual domain; hence, a total SF<53 was considered as impaired.
A trained interviewer conducted the interviews and assisted participants in completing the questionnaires when necessary, in a private room at the clinical center.
Descriptive statistics were performed to describe the variables of the patients, with frequencies and percentages for qualitative variables and the mean (x) and standard deviation (Sd) for quantitative variables. The characteristics of patients were compared considering diagnosis, sex, and age, using the Pearson-X² test and the Student’s t-test for qualitative and quantitative variables, respectively. Association between variables with total SF score, impaired SF, DSD in women, and ED in men was tested with the Mann-Whitney U Test or the Kruskal-Wallis ANOVA by Ranks (for quantitative variables), the Pearson’s-X2 test (for qualitative variables) and the Spearman-Rank correlations (high >0.8, average 0.5-0.7, and low <0.5). Simple linear or binary logistic regression analyses were performed for variables with a significant association in bivariate analysis. The univariate odds ratios (exp B) and confidence intervals (95 % CI) were computed for each analysis.
All statistical analyses were performed using SPSS (version 22.0, IBM Corp. USA). P-values <0.05 were considered statistically significant.
Results
Sociodemographic and health characteristics
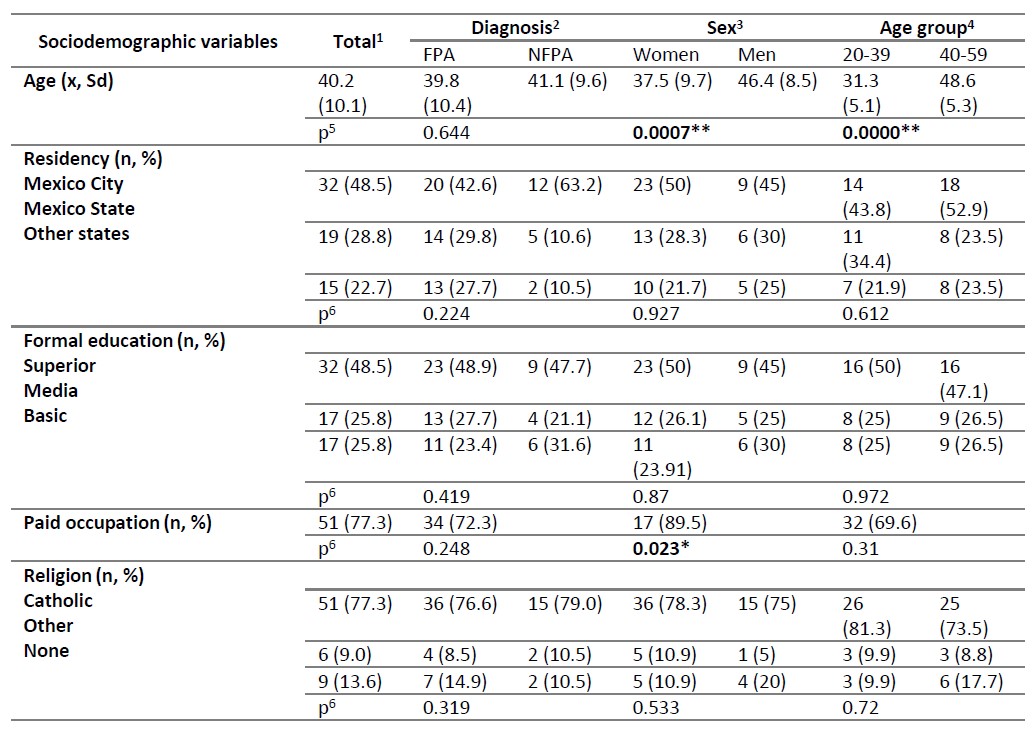
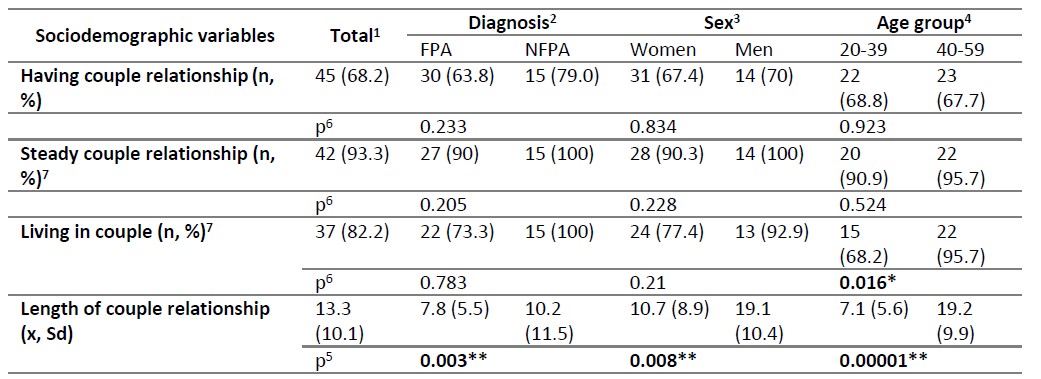
Patient sociodemographic characteristics and their comparisons between diagnosis, sex, and age group are summarized in Table A1. Sixty-six patients (46 women, 70 %, and 20 men, 30 %) participated in the study: 47 with FPA (72.2 %) and 19 with NFPA (28.8 %), 32 young adults (48.5 %) and 34 middle-aged adults (51.5 %). The mean age for the total sample was 40.2 ± 10.1 years, with men showing higher values. Most patients lived in Mexico City (32, 48.5 %), reported a superior level of formal education (32, 48.5 %), had paid occupations (51, 77.3 %), were mainly men, and referred being Catholic (51, 77.3 %). Most patients (45, 68.2 %) had a couple relationship, mainly steady (42,93.3 %), and reported living with the couple (37, 82.2 %). The mean of the length of the couple relationship was 13.3 ± 10.1 years, being higher in NFPA patients, men, and middle-aged adults.
Considering the type of secreting hormone in FPA, 15 patients (31.9 %) were diagnosed with CD (adrenocorticotropic hormone-secreting), 14 (29.8 %) with acromegaly (growth hormone GH secreting), 14 (29.8 %) with prolactinoma (PRL secreting), and 4 (8.5 %) as plurihormonal (GH and PRL secreting). According to the PA size, 25 patients (53.2 %) with FPA were classified with macroadenomas and 22 (46.8 %) with microadenomas, whereas 10 patients with NFPA (57.9 %) were classified with microadenomas and 9 (47.4 %) with macroadenomas.
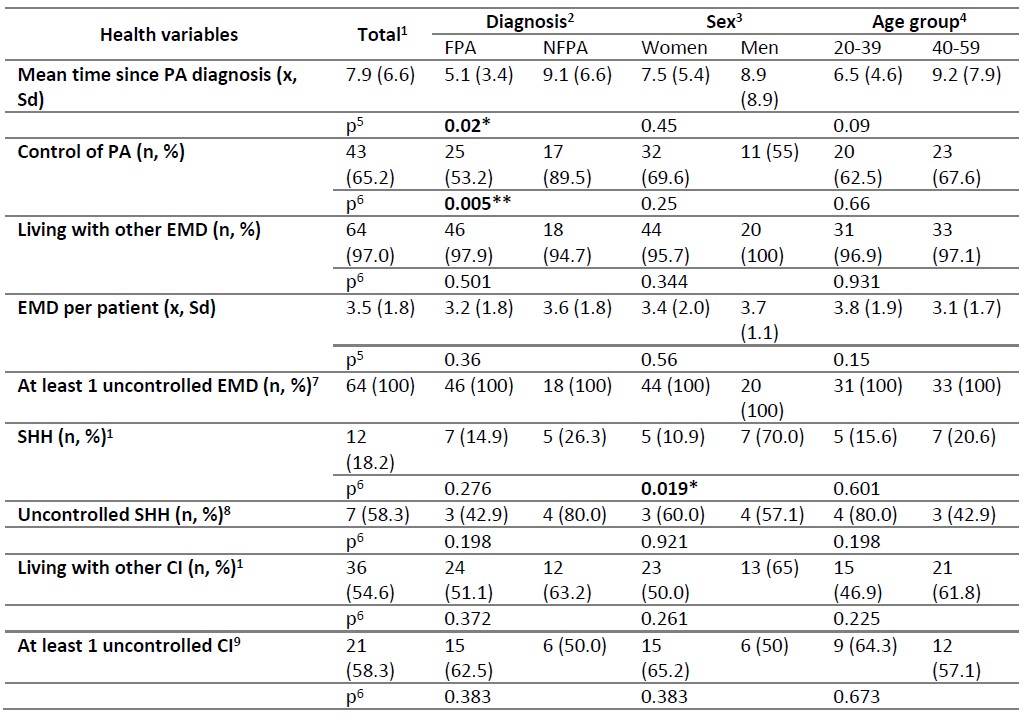
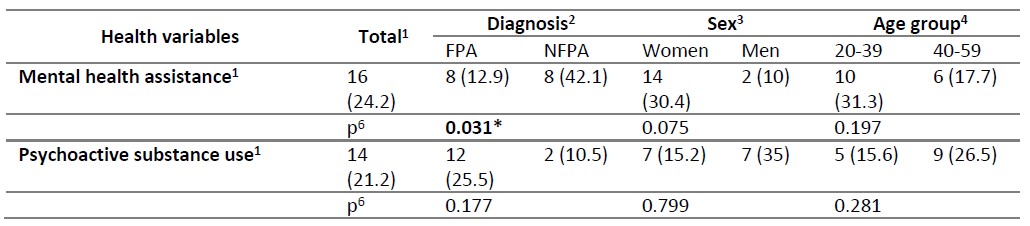
Patient health characteristics and their comparisons between diagnosis, sex, and age group are summarized in Table A2. The mean of time since the PA diagnosis was 7.9 ± 6.6 years, being higher in NFPA. Most patients (43, 65.2 %) were in control of the PA, especially the NFPA ones. Almost all patients (64, 97.0 %) had other endocrine and metabolic disorders (EMD), and all of them had at least one uncontrolled. The most frequent EMDs were dyslipidemia (42, 65.6 %), vitamin D deficiency (34, 54.7 %), thyroid disease (28, 43.8 %), insulin resistance (27, 42.2 %), and obesity (25,39.1 %). Twelve patients (18.2 %) had secondary hypogonadotropic hypogonadism (SHH), mainly men, and mostly (7, 58.3 %) were uncontrolled from this condition. More than half of patients (36,54.6 %) were living with other chronic illnesses (CI), and most of them (21, 58.3 %) had at least one uncontrolled. The most frequent CI diagnoses were digestive (19, 52.8 %) and cardiovascular (17,47.2 %). About a quarter of patients (16, 24.2 %) received mental health assistance, especially for depressive disorders (7, 43.8 %) and coping with conflict situations (6, 37.5 %), and a similar proportion (14, 21.2 %) used psychoactive substances, mostly cigarettes (8, 57.1 %) and alcohol (7, 50 %).
Sexual and reproductive health characteristics
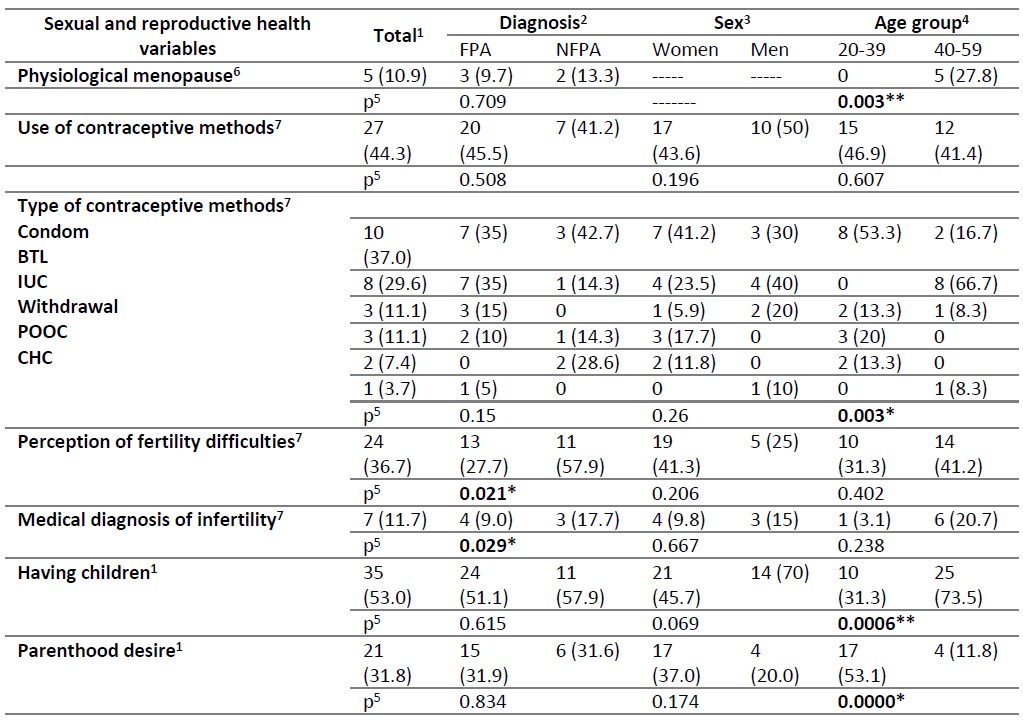
With regard to the RH variables, 5 middle-aged women (10.9 %) were in physiological menopause. They were excluded from the analysis of the following reproductive variables, except for the parenthood desire. Table A3 shows specific information about sexual and reproductive health characteristics. Less than half of patients (27, 44.3 %) used contraceptive methods, especially condoms (10, 37.0 %) by young adults and bilateral tubal ligation-BTL (8, 29.6 %) by middle-aged adults. More than a third (24, 36.4 %) perceived having fertility difficulties and 7 (11.9 %) had a medical diagnosis of infertility, mainly the NFPA patients. More than half of patients (35, 53.0 %) had children, mostly middle-aged, and around a third (21, 31.8 %) referred parenthood desire, especially young adults.
With regard to the SH variables, almost all patients identified themselves as heterosexuals (61, 92.4 %) and reported having initiated sexual intercourse (62, 93.9 %). Most patients referred current coital activity (45, 68.2 %) and more than a third (24, 36.4 %) reported autoerotic activity; hence, most (52, 78.8 %) participants reported being sexually active at the time of the study. Three patients (4.6 %) were infected with sexually transmitted infections-STI (all middle-aged men with FPA and HIV), and 27 (40.9 %) were considered to have sexual discomforts as DSD (10, 37.0 %), mainly in women, and ED in men (6, 22.2 %). Other sexual discomforts referred were pain/discomfort during coitus (5, 18.5 %), women referred self-limited sexual activity because of unsatisfied self-image (3 with FPA, 11.1 %), coitus absence, coital bleeding, difficulty in reaching the orgasm, couple conflicts with negative effects on the couple’s sexual performance, and health worries for the absence of sexual activity (1, 5.9 %, each one), and men referred decreased seminal volume (2, 7.4 %), an ejaculation, premature ejaculation, and increased sexual desire (1, 10.0 %, each one).
Assessment of the psycho-affective state and the sexual function
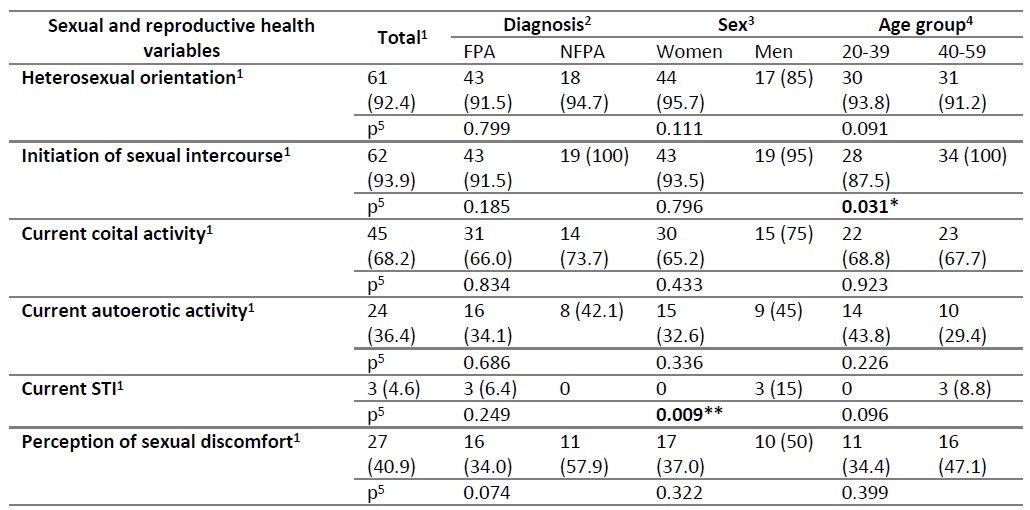
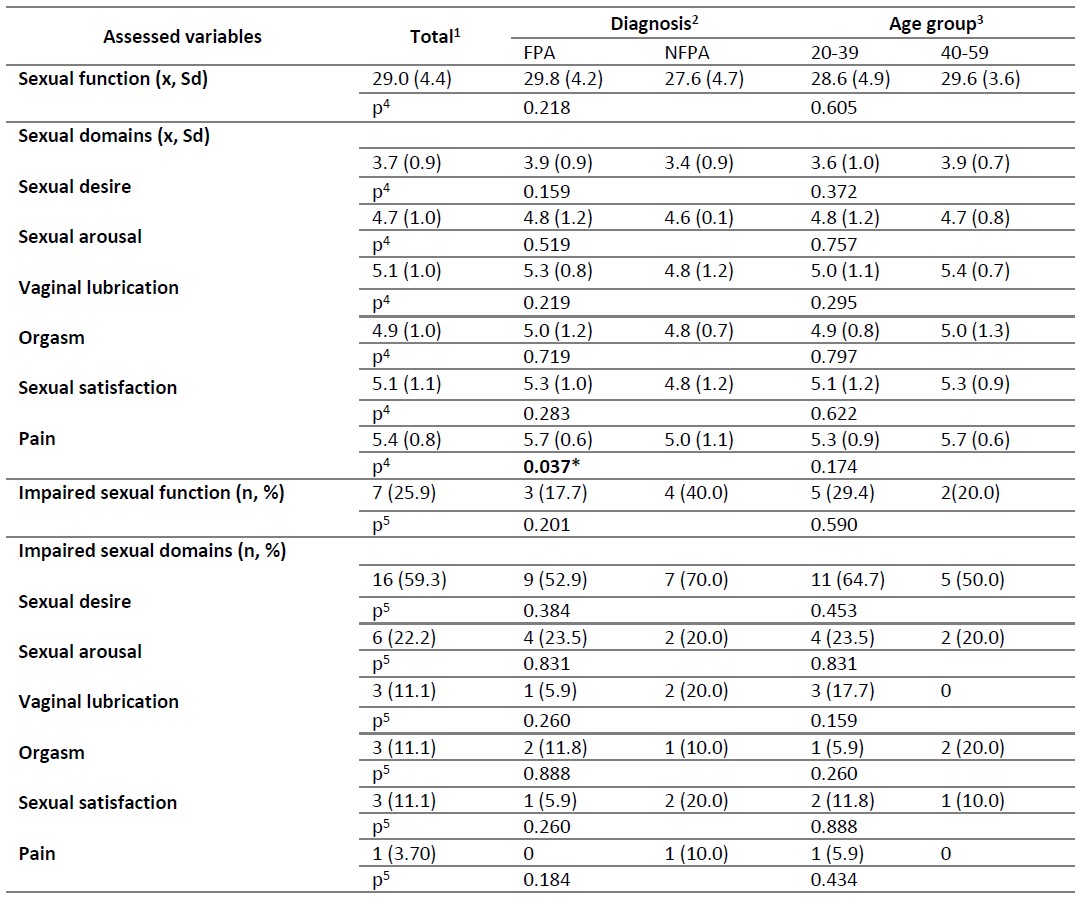
The results of the psycho-affective state assessment and their comparisons between diagnosis, sex, and age group are summarized in Table A4. Most patients (49, 74.2 %), generally women, scored with anxiety at a mild level (32, 48.5 %). The severity anxiety ranges showed significant differences considering the age group. Twenty-eight patients (42.4 %) scored with depression, mainly mild (13, 19.7 %) and moderate (11, 16.7 %).
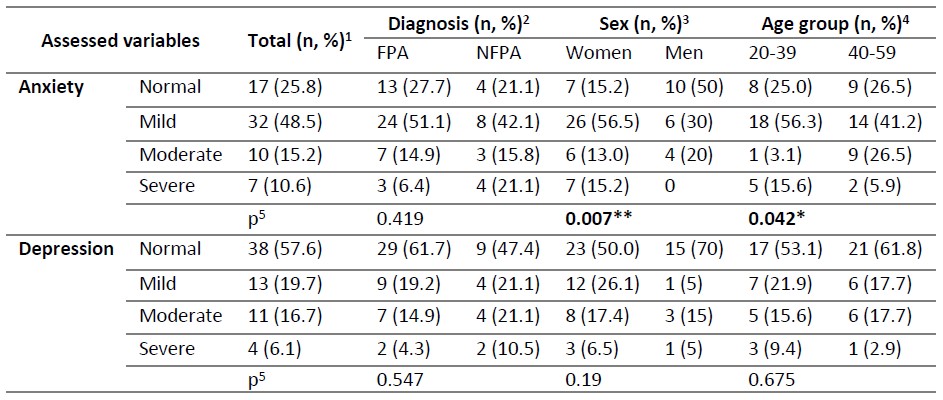
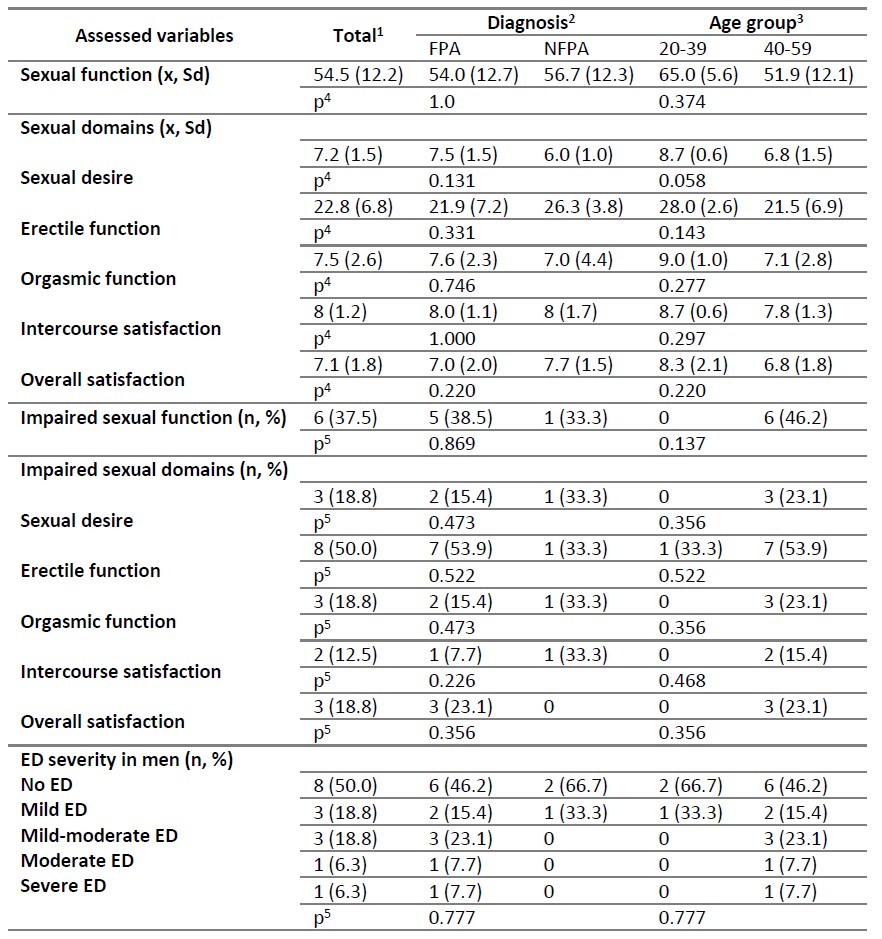
Most patients (43, 65.2 %) completed the SF questionnaires (27 women, 58.7 %, 16 men, 80 %). The results of the SF assessment and comparisons according to diagnosis, sex, and age group are summarized in Table A5 and A6. The mean of the total SF score was above the cut-off in women (29.0 ± 4.4) and men (54.5 ± 12.2), and a quarter of women (7, 25.9 %) and more than a third of men (6, 37.5 %) had scores consistent with impaired SF.
Almost all the mean scores of the female sexual domains surpassed the cut-off values, except for sexual desire (3.7 ± 0.9) in which more than half of women (16, 59.3 %) had scores consistent with impairing. The other female sexual domains showed frequencies of impairment under 23.0 %. The higher scores were obtained in the pain domain (5.4 ± 0.8) mainly in women with FPA. No significant differences were found in the total SF mean scores nor in the frequencies of the impaired SF or other female sexual domains.
Most of the mean scores of the male sexual domains surpassed the cut-off values, except for intercourse satisfaction (8.0 ± 1.2) and EF (22.8 ± 6.8), and half of the men (8, 50 %) showed mainly mild and mild-moderate ED (3, 18.8 %, each one). The other sexual domains showed frequencies of impairment under 19 %. No significant differences were found regarding the means of the total male SF scores and the sexual domain scores neither in the frequencies of impaired SF and impaired sexual domains.
Association analysis between some variables with the sexual function and with the presence of impaired sexual function
From the sociodemographic variables, it was found a negative and very low correlation between age and the SF score (p <0.05, r=-0.027), and an association between age with the impaired SF and ED in men (p <0.05). From the health variables, it was found an association between having SHH with the SF score and with the impaired SF in women (p <0.05), between living with other CI and the SF score, and between having at least one uncontrolled CI and the impaired SF, these last in men (p <0.05). From the SRH variables, there was a significant association between the perception of having sexual discomforts with the SF score, the impaired SF (p<0.01), and the DSD (p <0.05), and between the use of contraceptive methods with the impaired SF (p <0.05), all in women; whereas in men between the autoerotic activity with the impaired SF and ED, and between the perception of fertility difficulties with the SF score and with the impaired SF (p <0.05). It was found a negative and average correlation between anxiety (p<0.05, r=-0.614) and depression (p<0.05, r=-0.586) and the SF scores, an association between depression with the impaired SF, and an association between anxiety and depression with the DSD, all in women. In all cases, the correlations had p values <0.05, and the point value is shown in Table 1.
Table 1. Association between some sociodemographic, general health, SRH, and psycho-affective variables with the SF score, the impaired SF, and the decreased SD in women and ED in men
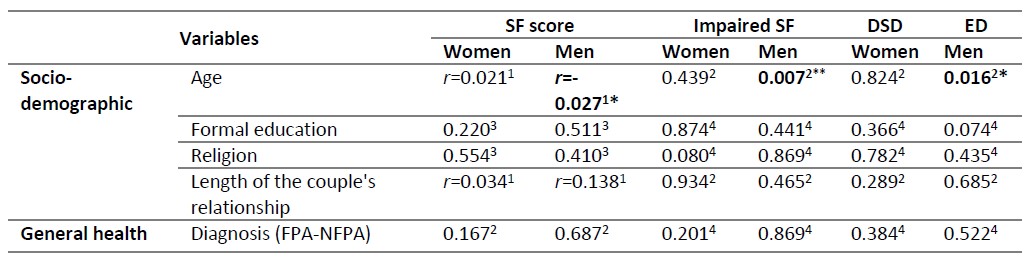
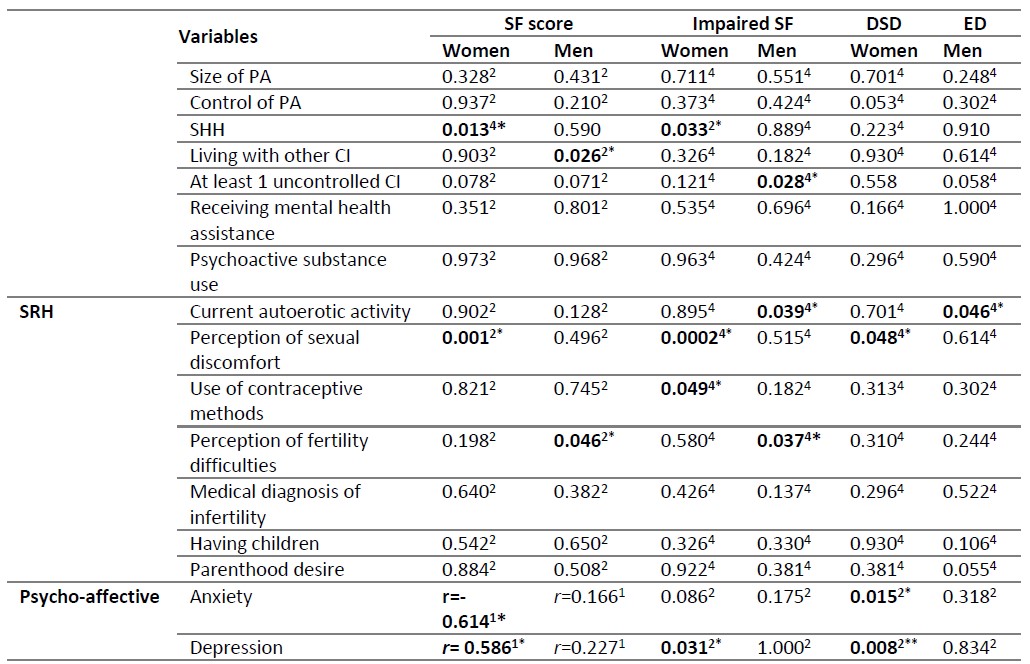
1 Spearman Rank order correlation. r: Spearman's coefficient: *p˂0.05.
2p value from Mann-Whitney U Test: *p˂0.05.
3p value from Kruskal-Wallis ANOVA by Ranks.
4 p value from Pearson’s Chi-squared test: *p˂0.05.
CI: chronic illness; DSD: decreased sexual desire; ED: erectile dysfunction; FPA: functional pituitary adenoma; NFPA: nonfunctional pituitary adenoma; PA: pituitary adenoma; SF: sexual function; SHH: secondary hypogonadotropic hypogonadism; SRH: sexual and reproductive health.
Source: Authors elaboration
Regression analysis from the associated variables with the sexual function and with the presence of impaired sexual function
As summarized in Table 2, the predictive variables that showed an effect on the decrease of the total SF score in women were the SHH diagnosis [adjusted R2 (AR2): 0.274; OR: -0.55 CI 95 % (-14.9_- 3.4)], the perception of sexual discomfort [AR2: 0.450; OR: -0.69 CI 95 % (-8.6_-3.4)], and the anxiety score [AR2: 0.171; OR: -0.45 CI 95 % (-0.3_-0.03)], all with low effects and p-values <0.05. In men, age showed a low effect on the decrease of the total SF score [AR2: 0.426; OR: -0.68 CI 95 % (-1.57_- 0.37); p=0.004]. The impaired SF, DSD in women, and ED in men had no predictor variables with significant regression coefficients.
Table 2. Regression analysis between the correlated variables with the SF score, the impaired SF, and with decreased SD in women and ED in men
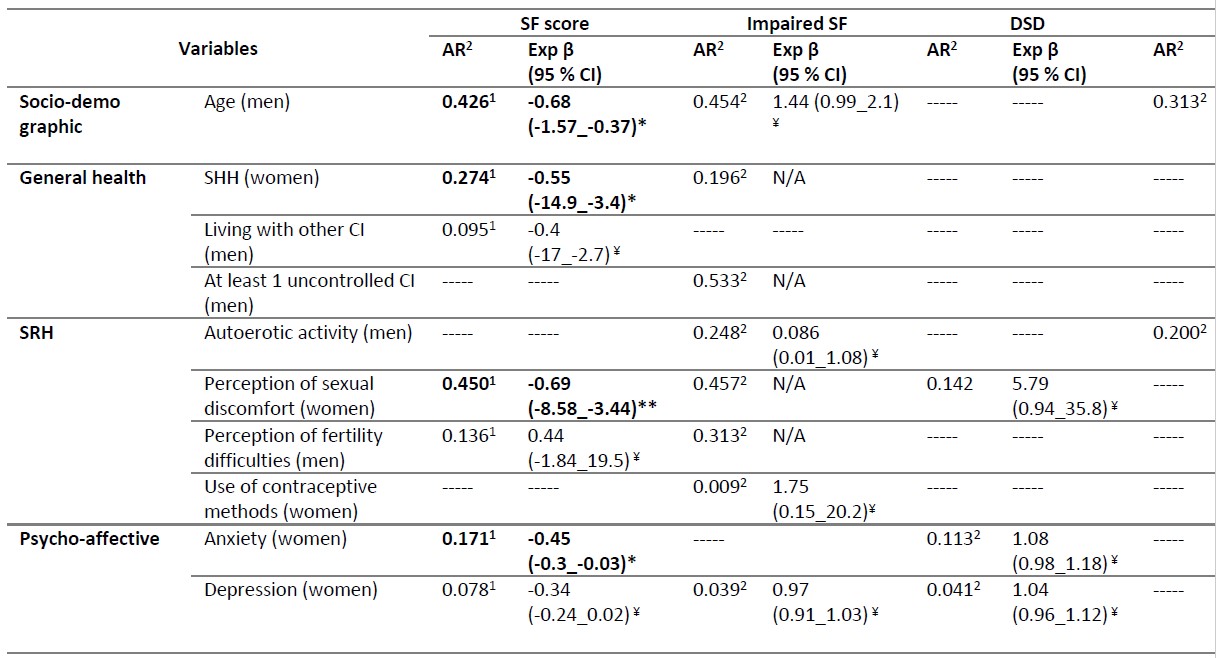
AR2represents the adjusted R2 from linear regression analysis1 and from binary logistic regression analysis2
* *represents p values from the significance of the regression analysis: *p˂0.05, **p˂0.01, ¥>0.05.
CI: chronic illness; DSD: decreased sexual desire; ED: erectile dysfunctions; N/A: Not applicable because OR could not be estimated due to frequencies equal to 0; SF: sexual function; SHH: secondary hypogonadotropic hypogonadism; SRH: sexual and reproductive health.
Source: Authors elaboration
Discussion
PA can influence the SRH through the features related to the disease itself, to the treatment, and to the associated psychological issues (Balercia et al., 2007; Novoa et al., 2013; Krysiak et al., 2016). Thus, the relevance of providing insight into the possible biopsychosocial factors related to SF in this population. The present study assessed SF in patients with PA and determined its relationship with some sociodemographic, health, SRH, and psycho-affective variables.
The mean scores in women exceeded the cut-off values for the total SF score and each sexual domain, with the exception of sexual desire which was the most vulnerable sexual domain in women with more than half of women with impairments. The better scores and the lowest frequencies of impairing were obtained in the pain, vaginal lubrication, and satisfaction sexual domains. These may express the relative structural and functional preservation of the sexual organs, the adequacy of the sexual arousal process (Lundberg & Hulter, 1991), and/or the positive effect of a satisfactory intimacy and couple relationship, aspects that were not explored. Some authors have identified impairing only in sexual desire (Krysiak et al., 2016), whereas others have found almost all sexual domains impaired (Granata et al., 2012; Celik et al., 2013), but sexual desire has consistently been recognized as the most affected domain in women with PA (Granata et al., 2012; Celik et al., 2013; Carosa, Sansone & Jannini, 2020).
In the men studied, the mean total SF score also exceeded the cut-off value and so did the sexual domain scores except for the intercourse satisfaction and the EF domains. The frequencies of impaired male sexual domains tended to be low except for the EF with scores consistent with ED in half of the men. Several studies also demonstrated the preponderance of ED in men with different PA (Buvat, 2003; Lotti et al., 2015; Wen-Jian-Long et al., 2018; Chen et al., 2019). Notably, the frequency of DSD in the men studied was not higher considering it is prevalent in patients with PA and could be associated with ED (Granata et al., 2012; Maggi et al., 2013; Wen-Jian-Long et al., 2018), as a result of the disease, the aging process, and the SHH diagnosis (Corona et al., 2016; Crawford & Kennedy, 2016).
These FSFI and IIEF findings were supported by the participants’ perception of having sexual discomforts, considered as sexual expressions that, although they do not constitute sexual dysfunction (SD) according to the clinical criteria (APA, 2013), have deleterious effects on sexual well-being from the subjective assessment (Alcántara-Zavala & Amuchátegui-Herrera, 2009). The DSD in women and ED in men are the most frequent sexual disorders in this population (Krysiak et al., 2016; Vieira-Cintra et al., 2018), the classic symptoms of severe hypogonadism (Balercia et al., 2007; Worsley et al., 2016), and have been associated to the psycho-affective dynamic of living with the disease and with the expression of traditional gender roles (Ledón et al., 2006; 2017). Other sexual discomforts reported also showed a sex divide with women referring discomforts in some biopsychosocial dimensions of sexuality (self-image, couple dynamics, overall health), while men are more restrained to the SF domains and to some of its biological aspects (seminal volume). To analyze these particularities some differences found in the studied women and men, about the age, the SHH diagnosis, and the psycho-affective state must be considered.
With regard to age, men not only showed a higher mean age than women, but correlation analysis indicated an inverse association between age and total SF score, and an association with the impaired SF and ED, whereas the regression analysis showed that age had a decreasing effect on the total SF score. Studies with patients with acromegaly have identified the aging process as associated with worse SF performances and SD (Celik et al., 2013; Vieira-Cintra et al., 2018; Chen et al., 2019). With regard to the SHH diagnosis, although most men were identified with SHH, there were women in whom the SHH showed an association with the impaired SF and had a predictive effect on the decreasing SF score. This makes it more striking that the mean scores of the other female sexual domains (besides sexual desire) were not lower. SHH resulting from disorders of the hypothalamus and pituitary gland causes a lack of sex steroid production and low serum testosterone levels (Barut et al., 2018; Richard-Eaglin, 2018). It is also associated with decreased HRQoL related to psychological effects (Flitsch, Spitzner & Lüdecke, 2000), and in women, SHH causes vaginal atrophy, reduced vaginal lubrication, discomfort during intercourse, and impair orgasm and satisfaction (Glasier et al., 2006). With regard to the psycho-affective state, women showed the highest scores of anxiety and depression, which inversely correlated with their SF score, showed association with DSD and with impaired SF in the case of depression, whereas the regression analysis showed anxiety as a predictor variable for the decrease of the female SF score. Studies have shown a high prevalence of psychological distress even in long-term cure pituitary disorders (Sonino et al., 2007; Cosci, Fava & Sonino, 2015), and inverse correlation between BDI and FSFI scores in this population (Celik et al., 2013; Krysiak et al., 2016; Vieira-Cintra et al., 2018). It is plausible to consider that the psycho-affective state in the studied women could explain why sexual desire was the most vulnerable female sexual domain, since it is closely related to psychosocial variables (Lightner, 2002; Celik et al., 2013), besides hormone deficiencies and medical intervention (Barut et al., 2018; Richard-Eaglin, 2018).
It is also possible that the particularities in the reported sexual discomforts and/or impaired sexual domains in women and men could also be explained by the traditionally gendered socialization that attributes different meanings to female and male sexuality. The values and principles of a patriarchal society are preponderant in Mexico, where sexual relationships are organized based on stereotypes assigned to each sex (Abril et al., 2018). The higher identification of the DSD in women and the ED in men could also express the relevance of the female availability for the sexual encounter as a subordination expression and the overvaluation of the sexual role of the penis as a male power extension, respectively (Sosa-Sánchez, 2013). These aspects were not explored in the study.
Other health and SRH variables also showed significant association with the SF indicators. In men, living with other CI was associated with the SF score, and having one uncontrolled CI was associated with impaired SF. Especially, ED is considered an early symptom of cardiovascular disease and other EMD due to common risk factors and pathophysiology mediated by endovascular dysfunction and chronic low-grade inflammation (Maggi et al., 2013; Lotti et al., 2015; Richard-Eaglin, 2018; Chen et al., 2019; Vargas-Ortega et al., 2019). In women, the perception of sexual discomforts predicted the decrease of the total SF score, which could express their awareness of their sexual vulnerabilities, whereas the use of contraception was associated with impaired SF. The research results about the effects of different contraceptive methods on female SF are controversial and seem to be more related to biopsychosocial and cultural variables (Casey, MacLaughlin & Faubion, 2016; Guida et al, 2019; Makhathini, Makinga & Green-Thompson, 2019). The autoerotic activity, a frequent sexual behavior in the male general population (Vilet & Galán, 2021), was associated with ED in the studied men and was associated with a lower risk of severe ED and DSD (Corona et al., 2010). The perception of fertility difficulties was associated with the SF score in men. Infertility has been considered a cause and a consequence of SD (Bechoua, Hamamah & Scalici, 2016), in part related to its psychological burden and its association with masculinity loss (Lotti & Maggi, 2018).
Different authors have documented the higher SF impact from FPA compared with NFPA, because of their hormonal effects and deleterious influence on psychosocial variables (Lundberg & Hulter, 1991; Lightner, 2002; Buvat, 2003; Balercia et al., 2007; Krysiak et al., 2016; Wen-Jian-Long et al., 2018). In the present study, there were not found significant differences in the sexual variables according to the diagnosis, except for the female pain domain, which scores represented the best sexual domain in FPA and NFPA. Finally, the frequency of impaired SF found in the third part of the sample is similar to the reported by some authors (Lotti et al., 2015; Vieira-Cintra et al., 2018), whereas others reported higher frequencies (Buvat, 2003; Granata et al., 2012; Celik et al., 2013; Chen et al., 2019). These relatively lower frequencies were congruent with the high sexual satisfaction found and may be related to the PA control in most patients and to other psychosexual variables such as the quality of the couple's relationship and sexual intimacy.
The present study has some limitations. The small number of the sample and the inter-groups, the sampling process, and the participation of a single clinical setting limited the generalization of the results. The cross-sectional design did not allow the establishment of a cause-effect relationship between the variables, and not comparing the results with a control group limited the understanding of whether they represented atypical characteristics of the group studied. The subjective nature of the information and the possibility that the sexuality topic may be considered taboo by the participants could generate recall errors and false negative responses. The different SF questionnaires for women and men limited the comparison according to sex. No assay was performed to determine the sexual hormonal status of the patients, and variables related to the couple’s relationship were not evaluated.
In conclusion, the SF of the assessed patients with FPA and NFPA showed a moderate performance based on the total SF mean score above the cut-off values on the identification of impaired SF in the third part of the sample and on the high sexual satisfaction in women and men. Some sex-related vulnerabilities were found in specific sexual domains, mainly DSD in women and ED in men. The female and male SF indicators considered showed an association and/or dependent relationship with some health, SRH, and psychological variables. These findings point out that patients with PA should receive physical and psychological support to improve their SF, from a multidisciplinary and gender approach. Further research is needed to expand the understanding of this topic.