CASE DESCRIPTION
Delusional parasitosis (DP), delusional infestation (DI) or Ekbom's syndrome is an uncommon but not rare 1-3 psychiatric disorder in which patients have a fixed, false belief that they are infected or infested with parasites or other living organisms 4-6. This condition may lead to self-mutilation 5 or affect other members of the family 7. It was first described more than a hundred years ago 8, and is classified as a persistent delusional disorder in ICD-10 9 or as a delusional disorder of the somatic type in DSM-V 10, although much is left to understand about this disease. The prevalence is estimated between 0.18 and 4.2 per 100,000 11,12, with an incidence of 1.9 per 100,000 12. However, its variation is wide: in the United Kingdom, the estimated incidence is about 4.9 per million 11.
Delusional infestation by proxy is estimated in approximately 5-15% of the cases 7,13. Its onset has been associated with changes in the glucose metabolism of the thalamus and the left putamen, and with alterations in the dopaminergic neurotransmission of the striatum, again in the left putamen 14. There is also evidence of abnormal frontolimbic brain activity 15 and abnormal grey and white matter volume 16,17.
It generally affects women over 50 (3060) years of age 6,18, with a mean age of onset at 56.9 years 19. It can be classified as primary or secondary; the primary form of the disease does not present an organic or psychiatric underlying cause (Table 1) 6,20,21, and patients are otherwise mentally healthy 6,22. A really uncommon form of this disease is DI by proxy, which is a shared psychosis referred as folie à deux or folie à trois, where patients believe that other individuals or pets are infested rather than themselves 18,23,24. This presentation is more frequent in veterinary practice 18.
Table 1 Drugs or conditions associated with the onset of secondary delusional infestation.
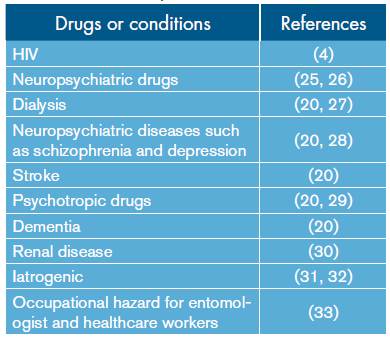
Source: Own elaboration based on the data obtained in the study.
The duration of the disease ranges from months to years 34. The most affected organ is the skin but other parts of the body can be affected as well 21,35. For its diagnosis, delusion must have a duration of at least 1 month, but patients must remain highly functional 1 and present with two main symptoms: 1) the strong belief of being infested despite medical evidence shows otherwise (100% of the patients), and 2) abnormal sensations as if an infectious agents caused them (88%) 6,36,37. Considering that the delusion of being infected can vary in intensity 38, in less severe cases the belief can be wavered but not reduced 39. Some of the symptoms reported are listed in Table 2 1,4,5,6,12,19,20,40,41.
Table 2 Possible symptoms of delusional parasitosis described by patients or relatives.
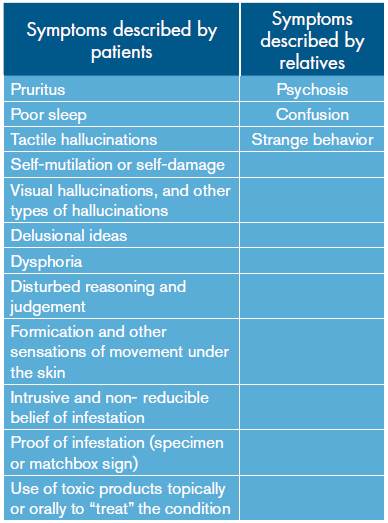
Source: Own elaboration based on the data obtained in the study.
Atypical manifestations appear when the "pathogens" are relatively large, the environment is infested rather than the individual, or the infestation is caused by inanimate objects 3,6,42. The infesting species range from unspecific living beings to microorganisms and small animals. These specimens can be "stored" and handled without disgust 6,43, and are treated as trophies instead; the specimen, however, should be examined 43. This is known as the "Matchbox sign", which is characterized by the patient collecting an inert substance (for example, dead skin) in a container, stating that it contains living specimens of the parasite in different stages of development 12.
The delusion can result in damage to the skin, hair, eyes and other family members, as they try to "clean" the infestation with dangerous substances or elements including fire and electricity 6,44,45. This condition can be affected by a large array of complications as listed in Table 3 6,12,35.
Table 3 Possible complications of delusional parasitosis
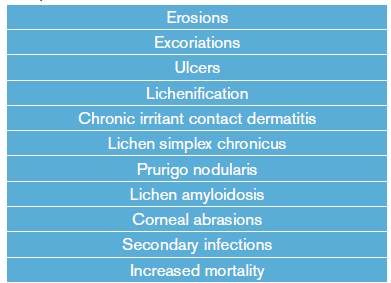
Source: Own elaboration based on the data obtained in the study.
The recommended treatments are based on anti-psychotic medication such as risperidone, pimozide 36,46, olanzapine, amilsupride, quetiapine and aripiprazole 47-50. Atypical anti-psychotics have a more favorable side-effect profile 50. The therapeutic effect may be observed between one to ten weeks 47. Lepping et al. 51 assessed the efficacy of this drugs, reporting that typical and atypical anti-psychotics achieved a remission proportion of 60-100%. In less severe cases, non-pharmacological treatment, such as psychotherapy, can be used 50,52. Other non-pharmacological therapies include: neurosurgery, transcutaneous electric stimulation and electroconvulsive therapy 50, with a less than optimal success rate 36,50.
Joint management by psychiatrists, psychologists and dermatologists is required 28,53-55, preferably in a clinic dedicated to psychodermatology 56,57. Adequate treatment leads to remission in 75% of the cases, although 25% of those patients may relapse and require longer therapy 58. Treatment should be introduced after obtaining a complete medical history and a systematic evaluation 54, specially to discard secondary causes or differential diagnosis 59-63 (Table 4). Offering antimicrobial or anti-parasitic drug trials reinforces the delusional ideas and is not recommended 6.
Table 4 Differential diagnosis of delusional parasitosis.
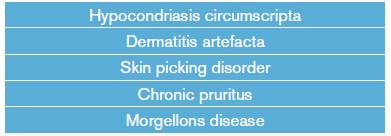
Source: Own elaboration based on the data obtained in the study.
Three groups of patients have been suggested for classification purposes: 1) patients with hypochondriac traits, 2) patients with paranoid symptoms and without hypochondriac apprehensions, and 3) patients with hypochondriac and paranoid traits 64. Most patients have other associated psychological disorders including anxiety, depression and appearance-related concerns, among others 37,65. More information can be obtained in the review made by Freudenman 6.
CASE DESCRIPTION
Female, 53 year-old, Hispanic businesswoman who attends, by her own volition and alone, an outpatient medical appointment at the Parasitology Department of Instituto Nacional de Salud (National Health Institute), referring a clinical history of 5 years characterized by the perception of macroscopic parasites that crawl over her body, biting her face, head and anterior thorax, and leaving white eggs which evolve to brown adults in about eight days. She also referred generalized pruritus and shows excoriations due to scratching (Figures 1 and 2), which she "treated" with Vicks Vaporub, domeboro (calcium acetate and aluminum sulphate), crotamiton and Canesten (clotrimazole) cream. At some point, she also used thinner and varsol to wash her clothes and skin.

Source: Own elaboration based on the data obtained in the study.
Figure 1 A. Front of the patient. The lesions can be observed in the cheeks, arms, and chest. B. profile of the patient portraying a close up of the cheek lesions. C. Back of the patient showing the extent of the lesions.

Source: Own elaboration based on the data obtained in the study.
Figure 2 A. profile of the patient showing the lesions on both cheeks B. picture showing some of the multiple lesions on the scalp.
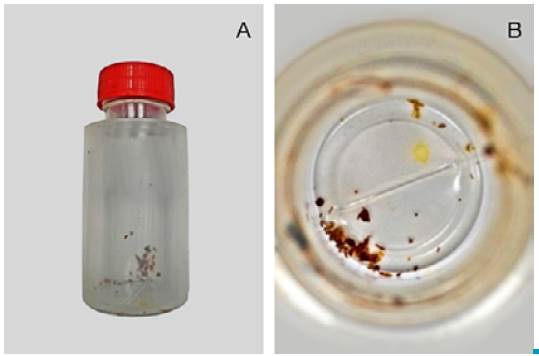
The patient takes to the appointment, in a small plastic jar, pieces of skin and coagulated blood which she says contain the eggs and two adults (Figure 3). This specimen is handled without disgust or contempt. She also describes how one of her sons have seen the parasites fly after one of the eggs hatched, while other members of the family do not have parasites but suffer from pruritus. Unfortunately, the relatives were not present during the interview and refused to be interviewed or examined afterwards, so this may be another delusory idea of the patient.
Source: Own elaboration based on the data obtained in the study.
Figure 3 A. Jar brought to the appointment by the patient. B. Close up of the jar contents.
She denies travelling to other places in the past five years. Medical background includes diabetes mellitus diagnosed twelve years ago, and pharmacological background includes metformin 850mg/day, glibenclamide 5mg/day, ivermectine 51 drops (which she has used in repeated doses since the onset of the disease), difenhidramine 50mg every 8 hours and, occasionally, amoxicillin 500mg every 12 hours; she denies using other medications. Her gynecological background is G4P3C0V3.
Physical examination revealed an arterial pressure of 100/60, heart rate of 84, respiratory rate of 18, temperature at 35.5°, weight 51.3kg, height 145cm, multiple excoriations on the scalp and neck, and cicatrized lesions in the inferior third of the face, chest and back. The patient had normo-reactive isocoria and eye bags; the rest of the physical examination was normal.
Regarding mental aspects, the patient had a negative attitude, was passive, cried easily, but had good visual contact with the interviewer. She had a slight psychomotor retardation and a sad attitude, with anxiety traits. Delirious thoughts were present, as well as sad mood, with semi-structured suicidal ideations, non-existent introspection, uncertain prospection, and good interpersonal relationships. Herspeech was not slurred, and her behavior was organized and non-catatonic. Even though she was depressed, she did not show any signs of alogia or affective flattening, and the depressive symptoms started long after the delusions. She did not hear voices.
Samples were taken, and cultures from feces and lesions were obtained, yielding negative results for microorganisms. Hemogram was normal, tests for liver and renal function were normal, and glycemic control was optimal. Toxicological exam was normal. Complete studies of the skin and fecal matter were made, yielding negative results as well. The specimens brought by the patient were analyzed providing a negative result. The patient was examined for needle marks which were absent. She did not present alterations in the rhinal mucosa nor respiratory or cardiac problems in the physical exam or medical tests.
Due to the absence of criteria to diagnose other psychiatric disorders or substance abuse or physical disease, the patient met the criteria of a delusional disorder of the somatic type (at least 1 month of delusions, visual hallucinations consistent with the disease, social function not markedly impaired, and brief mood episodes compared to the delusional period), thus Ekbom syndrome was diagnosed. The patient did not accept psychiatric treatment, and neither dermatology nor psychiatry services were able to assess the patient. Follow-up was not possible due to the refusal of the patient to start psychiatric treatment, even when it was suggested and advised for her depression.
Even though the patient did not accept treatment or referral, medical indications and recommendations were given. Prognosis is not optimal without pharmacological and dermatological follow-up or treatment, therefore, it is highly unlikely that the condition of the patient will be resolved.
Written informed consent was obtained from the patient for the publication of this case and the photographs.
DISCUSSION
Ekbom's syndrome, better referred as delusional infestation, is an uncommon disease that generally affects woman above 50 years of age. Physicians must be cautious when approaching this kind of patients, considering the words used and even the proposed therapies, in order to generate a good patient-physician relationship and help patients to understand the importance of treatment with a psychiatrist. Not conducting proper follow-up is dangerous; for instance, this case is a prime example of that, since the patient presented a typical primary delusional infestation that not only affects her life and self-esteem, but her family's life as well. Here, the information provided by the patient allowed to infer (although it was not confirmed) that some members of her family may suffer from delusional infestation by proxy. This presentation is similar to other cases reported in the literature 63.
Treatment is difficult and must be carried out based on an interdisciplinary approach. One way of improving treatment is through the use of psycodermathology, which is a new subspecialty emerging from dermatology, and includes interventions such as psychoeducation and cognitive behavioral therapy or joint interviews with dermatologists and psychiatrists 66 that have proven to be cost-effective 57.
Patients generally blame parasites, but can also consider other small organisms or inanimate objects. This condition can affect the individual, someone or something close to the individual or the environment, and there are even cases of shared psychosis.
Usually, sick patients are not violent, but they can be a threat to themselves and others since they may use dangerous substances during the "cleansing" process, and may even mutilate themselves. This case, as other cases 37, shows the relationship between underly ing psychiatric diseases and DI, and the long process involved to diagnose this disease. Physicians must first discard and find evidence that the patient is not infested, looking for symptoms or signs of underlying psychiatric disorders or the use of psychotropic drugs or conditions associated with this disease as well. Considerations about pets or individual victims of DI by proxy and their protection are outside the scope of this report.
Some of the most important aspects of this study include, first, initial assessment and referral, even though the patient did not follow the instructions, and second, the thorough clinical and physical examination alongside a complete laboratory analysis done to the patient. Some of the limitations are that the patient was never assessed by a specialist, that the outcome of the case is unknown, and that the relatives could not be evaluated, therefore, delusional infestation by proxy could not be confirmed.
CONCLUSION
This case clearly exposes the hardships of treating this type of psychiatric patients, as well as the difficulties for adequate follow-up and care. A better way of following and delivering care to these patients could possibly include domiciliary visits or clinics dedicated to psycodermatology. However, this case is important since it shows both classical and uncommon signs and symptoms, that the disease can affect patients and possibly their relatives as they can also suffer from similar symptoms (delusional infestation by proxy), and that they should also be included in the treatment. A comprehensive approach to the family and its involvement should be considered when approaching this type of patients.
PATIENT'S PERSPECTIVE
Follow-up was difficult, but during the few interviews that could be conducted, she expressed that her situation was dire, that she was desperate. Her mood had not improved and the negative thoughts were worse over time. At first, her work nor her relationships were affected, but they were compromised as the disease progressed, to such an extent that she was seeking advice from multiple physicians, but she thought that they did not believe her and never returned.














