Introduction
Open gastrectomy causes moderate-to-severe postoperative pain. Epidural analgesia has proven to be the technique of choice to control this pain.1 However, there are some contraindications or limitations for the insertion of an epidural catheter (coagulation disruptions, deformities of the thoracic spine, patient refusal), which mandates searching for an analgesic alternative. The introduction of ultrasound, as a work tool, has enabled the development of new regional anesthetic techniques for postoperative pain control. In this setting, the serratus-intercostal interfascial block or of the cutaneous branches of the intercostal nerves at the middle axillary line (modified BRILMA) was described in 2015, as an analgesic technique in patients undergoing open cholecystectomy.2 With the administration of the local anesthetic at the level of the 8th rib, into the fascial space between the anterior serratus muscle and the external intercostal muscle, it is possible to block the intercostal nerves T6 to 11, which are responsible for the innervation of the upper abdominal wall. Using an anesthetic-analgesic multimodal strategy with opioids, non-steroidal anti-inflammatory agents (NSAIDs), coadjuvants, and local anesthetics, the result is adequate control of postoperative pain, enabling an early recovery of patients. Patients undergoing open gastrectomy in whom a bilateral serratum-intercostal block was performed exhibited similar results to those of the immediate open cholecystectomy postoperative period.
Clinical cases
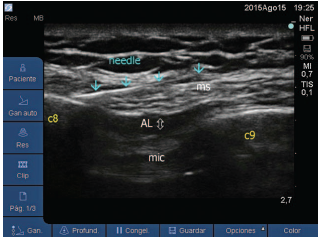
All patients described signed the informed consent prior to the administration of the anesthetic-analgesia technique in the series of cases (modified BRILMA). This fascial block in performed under ultrasound vision (M-Turbo portable equipment; Sonosite, Bothell, WA), using a 6 to 15-Hz high-frequency linear probe and an 80-mm Ultra-plex 360 needle (B. Braun, Melsungen, Germany). With the patient in supine decubitus, the probe is placed in the sagittal plane of the mid-axillary line (Fig. 1), to identify the fascial plane between the anterior serratus muscle and the external intercostal muscle. The needle is introduced from caudal to cephalic until the tip is placed at the level of the eighth rib, where 15 mL of levobupivacaine are administered into the fascial space, making sure that the agent is properly scattered (Fig. 2).
Case 1
A 62-year-old woman, American Society of Anesthesiologists (ASA) I, with a history of umbilical hernia repair, scheduled for laparoscopic gastrectomy. At her arrival to the operating room/operating theatre, the standard monitoring procedures were conducted (electrocardiography (ECG), pulse oximetry, and non-invasive blood pressure measurement), in addition to the Bispectral index (BIS; BIS VISTA monitoring system; Aspect Medical System Inc., Norwood, MA) to maintain an adequate depth of anesthesia. The patient was pre-medicated with 1 mg of midazolam and general anesthesia was induced with propofol 1.5 mg/ kg, fentanyl 150 mg, and rocuronium 0.6 mg/kg intravenous (IV) to facilitate orotracheal intubation. For maintenance of anesthesia, the necessary concentration of sevoflurane was used to maintain BIS values of 40 to 60. Due to the technical impossibility of introducing the laparoscopy trocars because of adhesions that developed following an old surgery, the surgical team decided to perform an open gastrectomy.
During the intraoperative period, the analgesia requirements were met with fentanyl boluses (500 mg in total). Before awakening, 50mg of dexketoprofene were administered and the bilateral modified BRIMLA block was performed.
Thepostoperativeanalgesicregimewassetat1gof paracetamol and 50mg of IV dexketopropofen every 8 hours and a rescue dose of 3mg of morphine in IV bolus in the presence of moderate-to-severe pain. Pain was assessed using the verbal numerical scale (VNS) with 0 (no pain) to 10 (the worst pain ever imagined), both at rest and dynamically (cough, deep breathing, moving). Moderate-to-severe pain was rated in VNS as greater than 5.
Once the patient was awake, she was transferred to a postanesthesia care unit (PACU). The initial evaluation showed a score of 9 in Aldrete scale and a VNS value of 1. A period of 2hours after admission to the PACU, the VNS score was 0 at rest and 2 in movement. At 8 hours, her assessment was VSN 1 at rest and 3 when breathing deeply. She required no rescue analgesia with opioids during her PACU stay and the patient was able to sit and ambulate over the first 48 hours.
Case 2
A 70-year-old male ASA II, programed for partial gastrec-tomy. The anesthetic-analgesia management in the OR was similar to that of the previous case. Some complications experienced during surgery required converting the laparoscopic approach to an open technique. An amount of 600 mg of fentanyl was administered intraoperatively. Before awakening, an ultrasound-guided bilateral fascial blockade of the serratum-intercostal plane was performed, to complement the multimodal intravenous strategy. The postoperative analgesia regime was identical to that of the previous patient. During the patient's stay in the PACU, pain was assessed according to VSN. At the time admission, the VSN score was 1 at rest; after 2hours, the VSN at rest was 2 and 4 with deep breathing. After 24 hours, when the patient tried to stand up, he experienced a VSN pain of 6, so 3mg of intravenous morphine was administered. The patient did not require any more opioid supplementation during his admission.
Case 3
A 41-year-old male, ASA I, with a history of neoadjuvant therapy for gastric cancer. The patient was programed for laparoscopic gastrectomy which was performed uneventfully. During the immediate postoperative period in the PACU, the patient became hemodynamically unstable and the computerized tomography scan (CT scan) confirmed hemoperitoneum, which led to reintervention with a midline laparotomy. The pain analysis showed a significant drop in hemoglobin, concurrent with coagulopathy. The OR protocol followed the guidelines previously described, except for a modified BRILMA block before the surgical incision. The analgesic demands were met with 300 mg of fentanyl. At admission to the PACU, once the surgery was completed, the VSN score was 0 at rest and in movement; therefore, no complementary analgesia with morphine was required.
Case 4
A 76-year-old male, programed for stomach laparoscopic surgery. The anesthetic approach was similar to that of cases 1 and 2 patients. The procedure was converted to open surgery because of significant bleeding. Over the 4 hours of the surgical procedure, fentanyl analgesia was administered on demand, up to a total of 600 mg. When the surgical procedure was over, and before the patient woke up, 50 mg of intravenous dexketopropophen was administered and the bilateral intercostal fascial nerves block was performed. The postoperative analgesic approach was similar to the previous cases. At admission to the PACU, the VSN at rest was 0 at rest. Pain intensity after 2 hours was 2 at rest, and 3 moving. However, after 8 hours, the patient complained of severe pain (VNS 6), so 3mg of intravenous morphine were administered. No additional opioid supplements were required during the postoperative period, and the patient was able to sit on a chair after 24hours of surgery.
Discussion
The most frequent problems following open gastrectomy are postoperative pain, the occurrence of nausea and vomiting, GI transit disruptions, cognitive dysfunction during the postop, and coagulation disorders/hypercoag-ulability.3 The search for an anesthetic-analgesic method allowing for a multimodal rehabilitation, that avoids these problems, has led to the design of a strategy that includes techniques based on the administration of local anesthetics, whether epidural, at the level of the fascial spaces, or into the surgical wound, with or without opioid supplementation.
Epidural analgesia has been the analgesic technique of choice to control pain following supraumbilical midline laparotomy, despite its contraindications or limitations, the proportion of failures, or the potential complications.4 Hence, in open gastrectomy, epidural analgesia is the best analgesic choice, superior to fascial blocks.5 Some alternatives have been assessed when the epidural cannot be administered, including intravenous lidocaine infusion; however, a Cochrane review failed to show superiority versus the epidural approach.6
The scientific evidence supports the use of multimodal analgesia as the technique of choice for abdominal surgery with midline incision.7 Each component of this strategy intends to raise the safety and effectiveness requirements. The analgesic approach must be performed taking into consideration that abdominal postsurgical pain has 2 components: somatic and visceral.
The skin, the muscles, and the parietal peritoneum of the anterior abdominal wall are innervated by the last intercostal nerves (T7-T11), the subcostal nerve (T12) and the first branches of the lumbar plexus (ilioinguinal and iliohypogastric nerves). The various techniques described in the literature for blocking of these nerves follow their anatomical path.8 Each intercostal nerve runs in antero-lateral direction, supplying a muscle branch, a subcostal ramus, and cutaneous rami, 1 lateral for the lateral segment of the thorax (T2-T6), and another 1 cutaneous anterior (between the internal oblique muscle of the abdomen and the transverse muscle) which ends in the posterolateral aspect of the rectus abdominis muscle and expresses the sensitivity of the anterior segment of the abdomen, innervated by the intercostal nerves T6 to T11. As the primary anterior divisions of the seventh to eleventh nerves run like the intercostal nerves until they pass behind the costal cartilages, it is then feasible to block 1 or several intercostal nerves along their path, to achieve analgesia of the upper abdominal segment.
The introduction of ultrasound has lowered the risk of blocks, increasing their effectiveness and adopting new approaches. The ultrasound-guided block of the trans-versus abdominis plane (TAP)9 was described in 2007, and its use in upper and lower abdominal surgery has grown since then. Subsequently, the same author introduces a change to the subcostal TAP. This is a fascial block in which the anesthetic is administered between the abdominis and transversus planes (subcostal TAP) to provide analgesia of the last thoracolumbar nerves. Although some trials show the superiority of epidural versus TAP10 in open gastrectomy, others fail to show any differences in the VNS at 72 hours, between both techniques, in supraumbilical surgery.11
There is a strong debate with regard to the dissemination and the maximum level achieved by the local anesthetic when administered as a single injection. The studies in this regard are not very conclusive, but point to the fact that the type of approach as a significant factor affecting the dissemination of the injected anesthetic, as the pharmacodynamics is disrupted, leading to differences in analgesia.12 A more posterior approach may lead to a sensitive blockade of higher dermatomes (T8) than the TAP (T10), in addition to a longer lasting analgesia, probably because of the blockade of the sympathetic ganglion inside the thoracic paravertebral space. Moving along with this theory, in supraumbilical surgery, the oblique subcostal approach would be the most appropriate, or the fascial blockade herein discussed, with an axillary midline approach.
As the intercostal nerves blockade (T2-T6) in the external fascial serratus anterior-intercostal space is effective for breast surgery, and the analgesia for open gastrectomy needs to reach a level below T6, in these cases of supraumbilical laparotomy we decided to do a blockade of the intercostal nerves at a more caudal level (T6-T11).
The intercostal nerves block into the serratus-intercostal space (BRILMA) is an interfascial blockade of the lateral and anterior cutaneous branches of the intercostal nerves in the axillary midline originally described under ultrasound in 2012.13 In this approach, the local anesthetic is administered to the plane between the medial aspect of the anterior serratus muscle and the external intercostal muscle, introducing a needle in plane, and placing the tip of the needle over the 4th rib. We introduced a change in 2015 which was the fascial blockade of the intercostal nerves T6 to 11 (modified BRILMA) as analgesic therapy in patients undergoing open cholecystectomy.2 This analgesic technique blocks the anterior cutaneous branches of the nerves T6 to 11, which although they are intermingled with the adjacent nerves, causing overlap of the innervation, this blockade is able to anesthetize the skin and the musculature of the abdominal wall. Visceral pain is managed with NSAIDs and paracetamol. Encouraged by the good results in these cases, we decided to use the technique in our 4 patients undergoing superior midline laparotomy.
There are no trials comparing this technique against epidural analgesia in open abdominal surgery, but there are studies on paravertebral blockade and blockade of the serratus-intercostal space in breast surgery14 where the technique offers an alternative to central blockade.
The results obtained have been evaluated as satisfactory in terms of pain control and low use of opioids, when doing the interfascial block of the intercostal nerves T6 to 11 (modified BRILMA) in open gastrectomy. This is an easy-to-perform blockade, with a smooth learning curve and few complications. However, well designed clinical trials are needed to compare this analgesic technique against epidural anesthesia, to be able to suggest it as an alternative in open gastric surgery.
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.











 texto em
texto em