Introduction
Worldwide, antimicrobial resistance has increased both in the hospital setting and in the community and this fact has been associated with decreased survival in specific populations.1 Beta-lactamases are the main mechanism of beta-lactam resistance in gram-negative bacteria.2 These enzymes cleave the beta-lactam ring producing inactive compounds by hydrolyzing most beta-lactam antibiotics, including penicillins; aminopenicillins; carboxypenicillins; ureidopenicillins; first, second and third generation cephalosporins; and occasionally, fourth generation cephalosporins.3
Klebsiella pneumoniae and Escherichia coli have been reported to be the most important gram-negative bacteria causing hospital-acquired infections, including urinary tract infection, pneumonia, and bacteremia. Moreover, it has been described that the presence of extended-spectrum β-lactamase (ESBL) production in these two germs is associated with increased mortality.4,5
Risk factors for the presence of ESBL-producing K. pneumoniae and E. coli in hospital settings include a history of antibiotic therapy, a history of hospitalization, duration of hospitalization, use of invasive devices such as central catheters or bladder catheters, chronic kidney disease, diabetes mellitus, and the presence of any anatomic or functional abnormality of the urinary tract.5-8
In the intensive care unit (ICU) setting, a relationship between the presence of ESBL-producing K. pneumoniae and E. coli and the development of bacteremia, urinary tract infection, intra-abdominal infection and pneumonia has been reported, which, in turn, is associated with an increased risk of mortality. Likewise, the use of central catheter, bladder catheter, mechanical ventilation; a history of use of antibiotics such as third generation cephalosporins; scores on disease severity scales such as the APACHE (Acute Physiology and Chronic Health Evaluation) II score; and length of stay in the ICU have been described as the main risk factors for the presence of this type of germs in the hospital setting, including ICU patients.7,9-13
In view of the above, the aim of this study is to determine the risk factors for healthcare- associated infections (HAI) due to ESBL-producing K. pneumoniae and E. coli in an ICU of a public tertiary care hospital and to evaluate the impact of this type of infection on mortality.
Materials and methods
Study design, study population, and sample
Retrospective case-control study with a 1:2 ratio. The study population comprised all critically ill adult patients (>18 years) admitted between January 2016 and December 2019 to the ICU (21 beds) of the Hospital de Kennedy, a public tertiary care hospital in Bogotá D.C., Colombia, and in whom a HAI (isolation) due to K. pneumoniae and/or E. coli was documented during their ICU stay (N=630). Sample size was calculated using the EPIDAT 4.2 software with an OR of 2.05, an alpha error of 0.05 and a statistical power of 0.8, resulting in a final sample of 97 cases and 194 controls.
The cases comprised patients with documented HAIs due to ESBL-producing K. pneumoniae and/or E. coli, and the controls included those with HAIs due to K. pneumoniae and/or E. coli with a natural resistance phenotype. The collection of cases and controls was completed in December 2019. It should be noted that the cases did not include patients in whom isolation of ESBL-producing K. pneumoniae and/or E. coli had been reported prior to admission to the ICU, nor those in whom this finding was documented 48 hours after admission.
Identification of ESBL-producing K. pneumoniae and E. coli isolates
The identification of ESBL-producing K. pneumoniae and E. coli isolates was carried out in an automated manner using a Microflex® LRF kit manufactured by Bruker. Subsequently, an antibiogram was performed and ESBL production was confirmed using the BD Phoenix® 100 automated microbiology system. Quality controls for the identification and susceptibility of microorganisms followed the recommendations of the Clinical & Laboratory Standards Institute (CLSI).
Variables
Information on the following variables was obtained by reviewing the medical records of each of the patients included in the study: age, sex, clinical severity according to the APACHE II score on ICU admission, cause of admission, blood creatinine level, presence of comorbidities (hypertension, heart failure, diabetes mellitus, etc.), requirement for mechanical ventilation, days on mechanical ventilation, presence and type of infection on admission to the ICU, antibiotic used in the ICU on admission, site of infection of the ESBL-producing germ, days of stay in the ICU, dialysis requirement, and mortality.
Statistical analysis
Categorical variables are described as absolute frequencies and percentages and continuous variables as medians and percentiles (p25-75), since the data showed a non-normal distribution (Shapiro-Wilks test).
Regarding the inferential analysis, a bivariate analysis was performed to determine the risk factors for HAIs due to ESBL-producing K. pneumoniae and E. coli: the chi-square test was used for categorical variables and the Mann-Whitney U test for continuous variables, since, as mentioned above, data in these variables had a non-normal distribution (Shapiro-Wilks test). A statistical significance level of p<0.05 was considered.
Finally, a multivariate analysis was performed in which the variables that obtained a p<0.1 in the bivariate analysis were entered into a logistic regression model. It should be pointed out that the variables "days of stay in the ICU" and "days on mechanical ventilation" were not included, as they could be confounding variables since they are both risk factors and consequences of infection by an ESBL-producing germ. A two-tailed test was performed with the p-values obtained and a significance level of p<0.05 was considered. All statistical analyses were performed in the SPSS software, version 26.
Ethical considerations
The study followed the ethical principles for conducting biomedical research involving human subjects established in the Declaration of Helsinki14 and the technical and administrative standards for health research contained in Resolution 8430 of 1993 issued by the Colombian Ministry of Health.15 In addition, it was approved by the Research Ethics Committee of the Subred Suroccidente de Kennedy, to which the Hospital de Kennedy adheres, as recorded in unnumbered minutes of April 10, 2015.
Results
ESBL-producing K. pneumoniae and E. coli isolates were identified in 57 (58.76%) and 40 (41.24%) patients, respectively, and these isolates were mainly obtained from urine samples (30.92%), followed by peritoneal fluid (27.83%). The median age of the participants was 54 years (p25-75: 30-68 years): 53 years in the control group and 55 years in the case group. Moreover, an APACHE II score >20 was obtained in 22.16% of the controls and 34.02% of the cases, and sepsis was the main cause of admission to the ICU in both groups (25.25% and 32.98%).
The presence of infection on ICU admission was reported in 52.06% (n=101) of controls and 73.20% (n=71) of cases; furthermore, the use of antibiotics on ICU admission was documented in 88.14% and 92.75%, respectively. Overall mortality was 28.17% (26.29% in controls and 31.95% in cases), but no significant difference was observed between groups (p=0.311). The clinical and demographic characteristics of the participants are listed in Table 1.
Table 1 Bivariate analysis of risk factors for healthcare-associated infection by extended-spectrum beta-lactamase-producing Klebsiella pneumoniae and Escherichia coli in patients admitted to the intensive care unit of the Hospital de Kennedy, Bogotá D.C., Colombia.
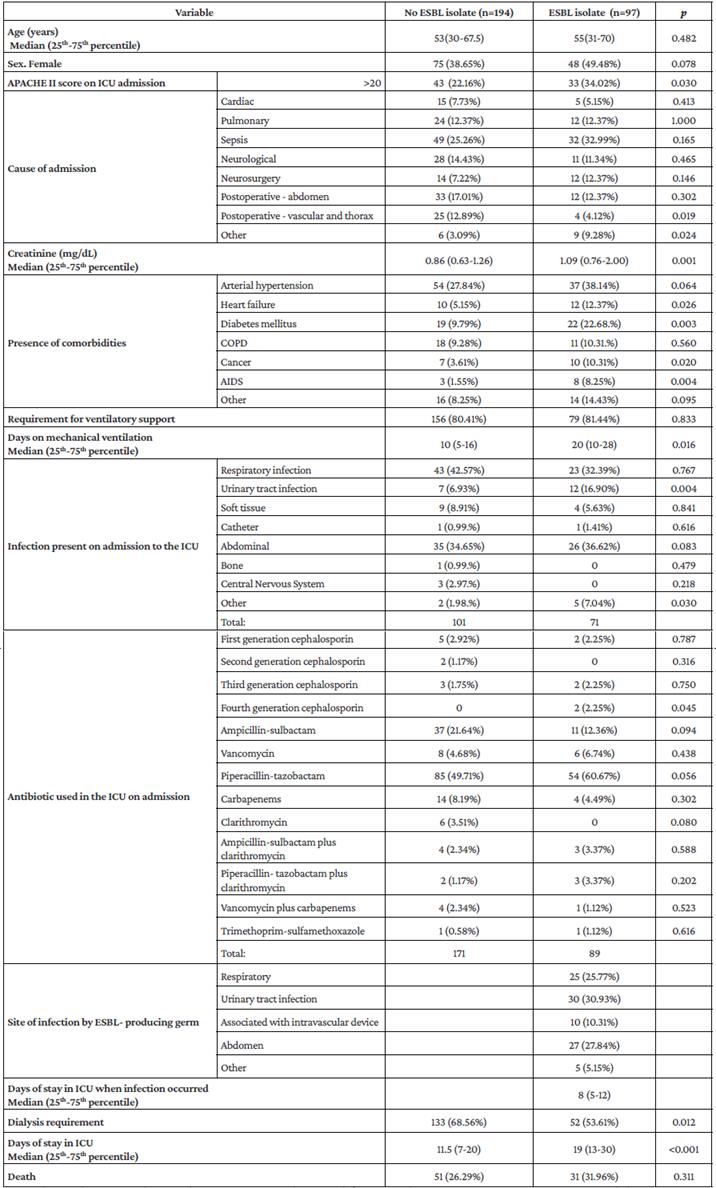
COPD: chronic obstructive pulmonary disease; AIDS: acquired immunodeficiency syndrome; ICU: intensive care unit; ESBL: extended-spectrum beta-lactamases.
Source: Own elaboration.
In the bivariate analysis (Table 1), it was found that, compared to the control group, the case group had a higher proportion of patients with an APACHE II score >20 (22.16% vs. 34.02%; p=0.03), the frequency of individuals with urinary tract infection on ICU admission was higher (6.93% vs. 16.90%; p=0.004), the proportion of patients requiring dialysis was lower (68.56% vs. 53.61%; p=0.012), and the median length of ICU stay was longer (11.5 [IQR: 7-20] vs. 19 days [IQR: 13-30]). There was no significant difference in the mortality rate between groups (26.29% vs. 31.96%; p= 0.311).
In the multivariate analysis (Table 2), urinary tract infection on admission to the ICU was found to be a risk factor for HAIs due to ESBL-producing K. pneumoniae or E. coli (OR=5.63, 95%CI: 1.918-16.527; p=0.002), with the clarification that the infection on admission was not caused by an ESBL-producing bacterium. In addition, dialysis requirement during the ICU stay behaved as a protective factor (OR=0.432, 95%CI: 0.246-0.756; p=0.003).
Table 2 Multivariate analysis of risk factors for healthcare-associated infection by extended-spectrum beta-lactamase (ESBL)-producing Klebsiella pneumoniae and Escherichia coli in the intensive care unit of the Hospital de Kennedy, Bogotá D.C., Colombia.
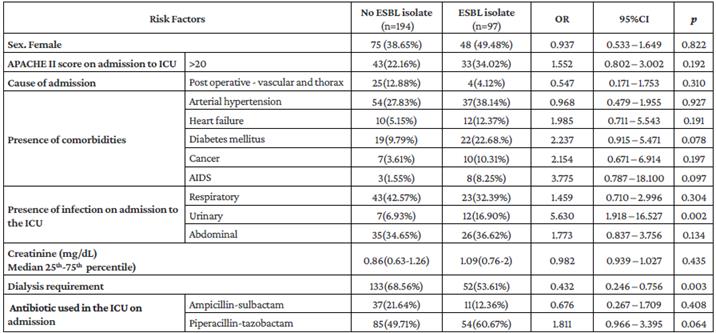
AIDS: acquired immunodeficiency syndrome; ICU: intensive care unit; ESBL: extended-spectrum beta-lactamases.
Source: Own elaboration based on the data obtained in the study.
Discussion
HAIs due to ESBL-producing enterobacteria are a serious problem worldwide both because of their high prevalence and because of the complications that derive from their presence, resulting in an increase in hospital stay and mortality risk.4,7-13 At the Hospital de Kennedy, where the present study was carried out, the prevalence of HAIs due to ESBL-producing germs have been increasing in recent years, so knowing the risk factors for this type of infection in the hospital is necessary to develop and implement an effective intervention to reduce their frequency.
In the present study, a statistically significant association was observed between having a urinary tract infection on admission to the ICU and the development of HAIs due to ESBL-producing K. pneumoniae and E. coli during ICU stay (OR=5.63, 95%CI: 1.918-16.527; p=0.002). In addition, dialysis requirement during ICU stay was found to be a protective factor for this type of infection (OR=0.432, 95%CI: 0.246-0.756; p=0.003).
In Colombia, several studies have been conducted to determine the risk factors for antimicrobial resistance in ESBL-producing E. coli and K. pneumoniae isolates in the hospital setting,10 including both patients admitted to the inpatient service and those hospitalized in critical care units.9,10 However, as of the date of this research, this is the first study in the country performed only with ICU patients, finding that the diagnosis of urinary tract infection on admission to the ICU was a risk factor for HAIs by this type of germs (OR=5.63, 95%CI: 1.918-16.53; p=0.002). This finding is similar to the one reported in the study conducted by Pineda et al.10 in patients treated in the hospitalization, emergency, intensive care and coronary care departments of two hospitals in Bogotá D.C. (555 patients: 185 cases and 370 controls), where the following risk factors for the development of urinary tract infection by ESBL-producing germs acquired in the community were reported: recurrent urinary tract infection (OR=2.13, 95%CI: 1.48-3.07), a history of chronic kidney disease (OR=1.56, 95%CI: 1.07-2.27), previous antibiotic use (OR=3.46, 95%CI: 2.48-5.35), recent hospitalization (OR=3.0, 95%CI: 1.96-2.45), a history of diabetes mellitus (OR=1.61, 95%CI: 1.06-2.45), and upper urinary tract infection (OR=2.64, 95%CI: 1.61-4.2).
On the other hand, in the multivariate analysis, dialysis requirement was a protective factor against the development of HAIs due to this type of germs (OR=0.432, 95%CI:0.246-0.756; p=0.003). This finding differs from the reports of different studies in which chronic kidney disease has been described as a risk factor for the presence of infections by ESBL-producing germs.9,10,16 In this regard, it should be noted that this discrepancy may be explained by the characteristics of the ICU in which the present study was carried out, since it is open and patients requiring this type of life-support therapy are treated in an environment with strict isolation parameters and, therefore, there are stricter asepsis and antisepsis measures.
The use of antibiotics such as piperacillintazobactam has been described as a risk factor for infection or colonization by ESBL-producing germs.13,17-19 In this regard, in the present study, although the multivariate analysis did not show a significant association between the use of this antibiotic on admission to the ICU and the development of HAIs due to ESBL-producing E. coli or K. pneumoniae during the ICU stay, this variable showed a tendency to behave as a risk factor, as was the case with the presence of diabetes mellitus.
Likewise, in the present study, no significant association was found between the presence of HAIs due to ESBL-producing E. coli or K. pneumoniae and variables that have been described as risk factors for infection by ESBL-producing germs. These variables include the use of cephalosporins12,13,16,20,21 (perhaps due to the limitation of their use in the Hospital de Kennedy by the institutional infection committee, which is reflected in the low frequency of use in both cases and controls), the severity of the disease20,22 (as determined by the APACHE II score on admission to the ICU), and the need for mechanical ventilation.19,20
Furthermore, it should be noted that our study did not evaluate variables that have been associated with this type of infection, namely, the requirement of a central catheter or bladder catheter22,23 (used in all of our cases and controls, which is why this variable was not considered), the use of antibiotics in the last 3 months, and a history of stay in a nursing home or receiving nursing care at home11,20,22,24-26 (variables that were not considered due to the unavailability of reliable data).
In the bivariate analysis, no statistically significant association was observed between the presence of HAIs due to a ESBL-producing germ (E. coli or K. pneumoniae) and mortality upon discharge from the ICU, a finding that has also been described in similar studies.12,24,27 However, there was a significant association with the variables days of stay in the ICU and days on mechanical ventilation, which has also been reported in the literature,19,20 with the median time in both variables being longer in the case group. It is important to highlight this fact, given its association, both causal and consequential, with infection by an ESBL-producing germ. In spite of the above, given the design of the present study, it was not possible to characterize them as independent risk factors, so they were excluded from the multivariate analysis due to the high risk of them being confounding variables.
Finally, as mentioned above, due to its methodological design, there were several limitations to the study that did not allow for a characterization of all the variables that, according to the relevant literature, are associated with antimicrobial resistance in ESBL-producing germs. Additionally, it should be noted that the ICU of the Hospital de Kennedy operates as an open unit where a higher risk of transmission of infectious diseases is expected, so it is not possible to extrapolate the findings reported here to the population treated in closed ICUs.
Conclusion
Urinary tract infection on admission to the ICU was a risk factor for HAIs due to ESBL-producing K. pneumoniae or E. coli, while the use of piperacillintazobactam on admission to the ICU and having diabetes mellitus showed a tendency to behave as a risk factor. Moreover, no significant difference was observed between cases and controls in terms of mortality. Understanding the risk factors for bacterial resistance allows the development of preventive, diagnostic and therapeutic strategies for its timely control. Consequently, further studies of this type are needed in order to obtain more data that will allow the development of predictive scales for HAIs due to ESBL-producing Enterobacteriaceae.















