Introduction
Bacterial resistance is a global problem which began naturally with the use of antibiotics. Resistant strains are increasing alarmingly worldwide. In Peru, there are descriptive studies such as the one carried out at Hospital Cayetano Heredia in 2017, which found a 28.6% preva lence of E. coli bacterial resistance to beta-lactamases. Ten years ago, the prevalence in the community was less than 5% 1.
Studies on the impact of the appearance of bacterial re sistance on patients, healthcare providers and the economic burden are heterogenous. One systematic review found that excess costs could be as much as 21,832 USD per patient, to more than 3 trillion USD in lost gross domestic product worldwide 2.
Urinary tract infection (UTI) is defined as the isola tion of a pathogen in the urine or leukocyturia, nitrites and/or bacteriuria on the urinalysis, together with urinary symptoms (dysuria, nocturia, frequency, cloudy urine) 3. Urinary tract infections can be classified as lower tract infections or cystitis, which are usually mild, and upper tract infections which entail greater severity and need for hospitalization (pyelonephritis) 3. Severe UTIs account for 13% of healthcare episodes in countries like the United States. Severe UTI is the second most frequent cause of infection in humans, after upper respiratory tract infections 4.
Escherichia coli is the most frequently found mi croorganism in UTIs and is responsible for 80-90% of community-acquired infections and 30-50% of nosocomial infections. It is also known that 25% of women with UTIs will have another episode within the next six months 5.
Extended-spectrum betalactamase (ESBL)-producing bacteria are resistant to penicillin and cephalosporin-derived antibiotics which have beta-lactam rings in their structure. Betalactamases are coded for by gene families known as TEM and SHV, and others such as CTM-X have recently been discovered, with as many as 95 known variants. Betalactamases have been found in strains of E. coli, Klebsiella spp. and Enterobacter spp., although also in non-fermenting microorganisms like Pseudomonas aeruginosa 6.
The objective of this study is to determine the risk factors for bacterial resistance in patients hospitalized for ESBL-producing Escherichia coli urinary tract infections, considering that it is an increasingly prevalent problem and the differences and risk factors in the literature must be determined to then propose interventions.
Materials and methods
An observational, analytical, case-control study. The clinical charts of adult hospitalized patients over the age of 18 who were hospitalized in the medical wards of two private clinics in the city of Lima (Clínica Ricardo Palma and Clínica Good Hope) with a discharge diagnosis of ESBL E. coli urinary tract infection (CIE-10: N39.0) during 2018- 2019 were reviewed.
The study hypothesis was the following: in hospital ized patients, are the prior use of antibiotics, prior UTIs, comorbidities, prior hospitalization, age and sex risk factors for ESBL E. coli UTIs? Are there differences with what is reported in the literature? (The null hypothesis being that there is no association.)
Cases were defined as the clinical charts of patients hos pitalized in the medical ward with a diagnosis of ESBL E. coli urinary tract infection confirmed by a urine culture taken on admission. Controls were patients hospitalized in the medical ward for any reason. These were controls because they shared the same characteristics of age, sex and having been hospitalized on the medical ward.
Cases were identified when patients were admitted to the medical ward with a diagnosis of pyelonephritis plus a positive urine culture for ESBL-producing E. coli recorded in the medical chart and at least one of the following signs or symptoms: dysuria, urgency to void, increased frequency, pelvic pain, flank pain, vesical tenesmus or fever or chills. A urine culture was considered positive when the bacterial count was greater than 105 colony forming units (CFUs)/mL in a sample of urine. Sensitivity tests and ESBL organism identification were performed by laboratory staff, as they have an automated VYTEC II system which generates a report showing the presence of betalactamase-producing resistance genes. None of the patients was using a urinary catheter on admission.
Once a case was identified, 1:1 pairing was performed with a patient hospitalized on the medical ward with the same demographic characteristics (age and sex).
Patients with the required data in the clinical chart were included. Patients with active pregnancy or with a permanent Foley catheter were excluded.
Age groups were classified as over or under 60 years old. Prior antibiotic use was defined as use from 24 hours up to six months prior to hospitalization. Hospitalizations up to one year prior to the current episode were taken into account. A UTI was considered to be recurrent when the patient had had at least one other urinary tract infection within the last six months. Comorbidities included any of the following conditions: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, connective tissue disease, mild or moderate liver disease, diabetes, hemiplegia, chronic kidney disease (moderate or severe), neoplasms, leukemias, malignant lymphomas, solid me tastases or HIV infection.
Data analysis
Statistical analysis was performed using the Stata 11.0 program, to determine association using a clinically signifi cant Chi2 (p<0.05), the degree of association using the odds ratio, and 95% confidence intervals. The associated factors with a p<0.05 in the bivariate analysis were included in the multivariate analysis according to the conditions of the logistic regression model.
The sample size (n=30) was calculated based on the literature for an approximate OR value of 8.7 15, with a frequency of exposure in the cases (P1) of 54% and in the controls (P2) of 18%. Applying the Epi Info 3.5.3 program, a sample of 28 cases and 28 controls is needed to obtain an OR of 8.7 with a confidence level of 95% and a power of 80%.
Ethical considerations
The study was initially approved by the Ethics Com mittee of the Universidad Cayetano Heredia School of Medicine, and by the research committees of both clinics. The clinical charts of incident cases of patients hospital ized on the medical ward with a diagnosis of complicated ESBL E. coli urinary tract infection (pyelonephritis) were reviewed. Likewise, controls were recruited from patients hospitalized on the medical ward.
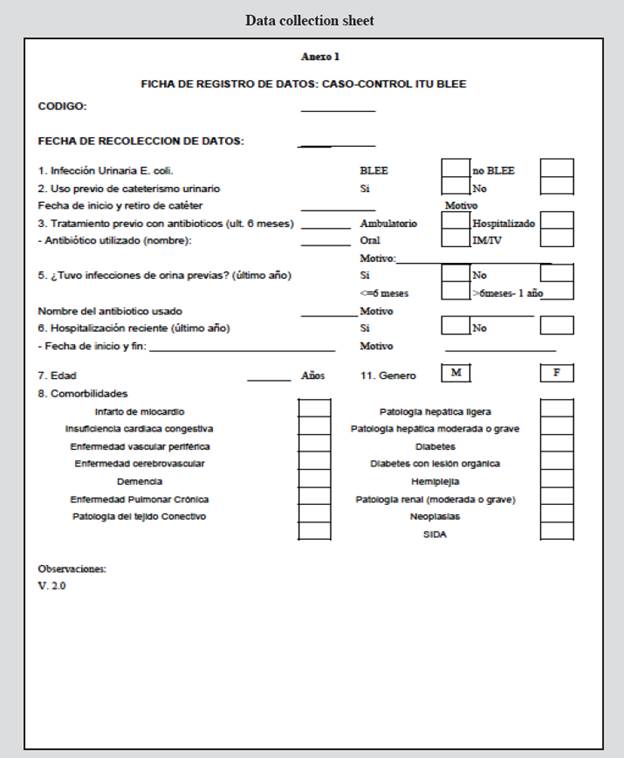
A form was used to collect the data from the clinical chart (Annex 1), for which a code was created to conceal the patients' identity; this code was also placed on an other worksheet along with the clinical chart numbers, to which only the investigator had access. This ensured data confidentiality.
Results
The average age of the cases was 72.4+16.9, and of the controls was 76.16+19.2. In the group of cases, 73.3% were over the age of 60, while 83.3% of the controls were over this age. Males made up 36.7% of the group of cases and 43.3% of the group of controls. There was no statistically significant difference in age or sex. In the group of cases, the most common prior antibiotics were second and fourth-generation cephalosporins, quinolones and nitrofurantoin.
The following variables were included in the bivariate analysis: age, sex, prior use of antibiotics, history of urinary tract infections and comorbidities. The last variable was divided into two categories: none or one or more comor bidities (Table 1).
Table 1 Risk factors for ESBL E. coli UTIs.
| Risk factors | Cases | Controls | Total | OR | 95%CI | X2 | p | |
|---|---|---|---|---|---|---|---|---|
| Prior antibiotic use | Yes | 29 | 3 | 32 | 261 | 22.5-11,017 | 45.27 | 0.000 |
| No | 1 | 27 | 28 | |||||
| Prior urinary tract infection | Yes | 24 | 3 | 27 | 36 | 6.97-227.24 | 29.7 | 0.000 |
| No | 6 | 27 | 34 | |||||
| Sex | M | 11 | 13 | 24 | 0.76 | 0.24-2.41 | 0.28 | 0.590 |
| F | 19 | 17 | 36 | |||||
| Age | <60 | 8 | 5 | 13 | 0.55 | 0.12-2.26 | 0.88 | 0.350 |
| >=60 | 22 | 25 | 47 | |||||
| Prior hospitalization | Yes | 21 | 10 | 31 | 4.67 | 1.39-16.04 | 8.08 | 0.005 |
| No | 9 | 20 | 29 | |||||
| Comorbidities | None | 15 | 19 | 34 | 0.58 | 0.18-1.83 | 1.09 | 0.290 |
| 1 or more | 15 | 11 | 36 | |||||
A logistic regression with the significant variables (prior antibiotic use, prior urinary tract infections, recent hospitalization) showed that only the use of antibiotics was statistically significant (Table 2).
Table 2 Logistic regression of the risk factors for ESBL E. coli UTIs.
| Risk factors | OR | Standard Error | z | P>|z| | [95%Conf. Interval] |
|---|---|---|---|---|---|
| Prior antibiotic use | 97.73 | 121.98 | 3.67 | 0.000 | 8.47 - 1,128.29 |
| Prior urinary tract infection | 6.49 | 7.20 | 1.68 | 0.092 | 0.74 - 57.14 |
| Prior hospitalization | 2.90 | 3.29 | 0.94 | 0.349 | 0.31 - 26.95 |
Discussion
The study highlights the importance of identifying the prior use of antibiotics as a risk factor for bacterial resistance, as it was the only factor which increased the probability of an ESBL E. coli UTI with a statistically significant difference and a significant magnitude on multivariate analysis.
The study population is older adults, with the overall proportion of those over 60 being 73.3% for cases and 83.3% for controls, with no difference in sex; therefore, the find ings should be interpreted in this context. According to the literature, as age increases, the prevalence of UTIs equalizes between men and women. Increased life expectancy and the increased risk of hospitalization for infections in older adults explains these proportions.
Regarding the prevalence of antibiotic resistance in E. coli urinary tract infections, a prospective multicenter study in the United States to evaluate the occurrence of E. coli urinary tract infections found that 3.9% of the isolated samples were ESBL E. coli; of these, 55% were community-acquired 7. Other similar studies in Spain, performed by a research group devoted to studying the sensitivity of ambulatory urinary pathogens, found a 5.2% prevalence of ESBL E. coli in 2006, which rose to 8.8% in 2012 8,9. In Peru, a study of ambulatory patients found that 16.3% of 325 E. coli isolates were confirmed to be ESBL producers 10,11. These figures reflect the alarm ing growing tendency towards increased E. coli antibiotic resistance worldwide.
Concerning the risk factors for acquiring ESBL E. coli, the studies agree on some very important factors such as prior hospitalization, the prior use of antibiotics, especially beta-lactams and quinolones, and gastrointestinal coloniza tion with ESBL-carrying strains 12,13. Other studies also describe other factors such as diabetes mellitus, recurrent UTIs, age over 60 and male sex 14.
Other diseases besides those mentioned above, such as heart failure, malignancy, liver disease and immunosuppression also cause a 2.6 to 6-fold increase in the risk of contracting a urinary tract infection caused by a resistant organism 15. The prior use of antibiotics (quinolones), use of urinary catheters, prior UTIs and recent hospitalization are associated factors with a significant magnitude (OR: 8.7, 6, 3 and 2, respectively) 16,17.
A study in Spain published in 2006 with 19 recorded cases of patients with community-acquired ESBL E. coli (with an average age of 61 years), found on multivariate analysis that exposure to second-generation cephalosporins was the only factor significantly associated with the de velopment of resistance (OR: 21.42; 95% CI: 5.38-85.22; P < 0.05) 18.
A case-control study in Pennsylvania of 33 cases with ESBL E. coli or ESBL K. pneumoniae and a similar age to our study found that the only factor in the multivariate analysis was the length of antibiotic therapy (OR for each day of antibiotic therapy: 1.10; 95% CI: 1.03-1.18; p<0.006). This study concluded that the antibiotic load was the only factor associated with bacterial resistance 19.
In both studies, both the prior use of antibiotics as well as the length of treatment increased the risk of bacterial resistance.
A study in 2013 also found other risk factors such as recent travel to Asia or Africa (OR: 21, 95% CI: 4.5-97), prior use of quinolones (OR:16, 95% CI: 3.2-80) and dia betes mellitus (OR:3.2, 95% CI:1.0-11). Travel tends to foster genetic exchange among bacteria, especially tourism in developing countries 20.
Another study in New Zealand in 2015, with 76 cases over the age of 65, found that the main risk factors associ ated with ESBL E. coli were: people residing in a nursing home and the prescription of antibiotics in a hospital (OR: 5.6; 95% CI: 2.5-12.9). When the OR for the prior use of any antibiotic is calculated, the result is also significant (OR: 20.96, 95% CI:8.94-43.59) 21.
In Japan, the final model of a retrospective case-control study published in 2016, in which 53% of the cases were over the age of 65, found that the independent risk fac tors for ESBL E. coli UTIs were male sex (OR:0.39, 95% CI:0.24-0.65), major surgery within the previous 60 days (OR: 2.89, 95% CI:1.54-5.30), prior use of tetracyclines (OR: 2.89, 95% CI: 12.58-57.28), second-generation cepha losporins (OR:3.04, 95% CI:1.48-6-07) and fourth-gener ation cephalosporins (OR: 50, 96% CI:27.51-94.18) 22.
The importance of new, emergent strains, including MDR ESBL E. coli, and the role of prior antibiotic use as a risk factor was also shown in recent studies in Korea in 2017, which found that the prior use of quinolones (OR: 15.53; 95% CI: 2.86- 84.27) and nosocomial infections (OR: 5.98; 95% CI: 2.26-15.86) were the main risk factors for resistance 23.
The studies of the most important risk factors for ESBL E. coli urinary tract infections are summarized in Table 3.
Table 3 Case-control studies of the risk factors for ESBL E. coli UTIs.
| Author | Year | Cases | Controls | Risk factor | OR 95% |
|---|---|---|---|---|---|
| Castillo-Tokumori F | 2017 | 67 | 105 | Prior antibiotic use Prior hospitalization Prior surgery Use of corticosteroids | 3.09 (1.42-6.74) 2.92 (1.29-6.62) 2.75 (1.94-8.03) 24.3 (2.39-246.9) |
| Park SY | 2017 | 30 | 100 | Prior antibiotic use Nosocomial infection | 15.53 (2.9-84.3) 5.98 (2.3-15.9) |
| Nakai H | 2016 | 33 | 647 | Male sex Major surgery within the last 60 days Prior tetracycline use Second-generation cephalosporins Fourth-generation cephalosporins Prior tetracycline use Second-generation cephalosporins Fourth-generation cephalosporins | 0.39 (0.24-0.65) 2.89 (1.54-5.30) 2.89(12.58-57.3) 3.04 (1.48-6-07) 50 (27.51-94.18) |
| Ikram R | 2015 | 76 | 156 | Prior antibiotic use (hospital, other indication) Dependence Female | 5.6 (2.5-12.9). 20.96 (8.9-43.6) 7.5 (2.2-25.7) 3.2 (1.5-6.9) |
| Soraas A | 2013 | 100 | 190 | Prior antibiotic use (quinolones) Travel to Asia or Africa Diabetes mellitus | 16 (3.2-80) 21 (4.5-97) 3.2 (1.0-11) |
| Calbo E | 2006 | 19 | 55 | Prior antibiotic use (cefuroxime) | 21.42 (5.4-85.2) |
Our results are consistent with the findings of a case-control study conducted at Hospital Cayetano Heredia in 2017, which found a significant association with the prior use of antibiotics (OR: 3.09, 95% CI 1.42-6.74). In this retrospective study, the cases were ambulatory urine cul tures with community-acquired ESBL E. coli urinary tract infections, and the controls were those with urine cultures with non-ESBL germs24. They are also consistent with other studies performed at the same hospital 25,26.
In summary, most of the risk factor studies come to the same conclusion as our study, that the prior use of antibiotics is a critical risk factor for bacterial resistance in urinary tract infections. Our study also has a strength in that the cases were incident hospitalized patients, that is, those with clinically relevant infections with regard to severity and higher associated costs.
The selection of controls is a study limitation because not all of these patients had a non-ESBL E. coli urinary tract characteristics with regard to age, sex and being hospitalized were also included; most of them had non-ESBL urinary tract infections, but not necessarily all of them. The design could be improved in future studies using controls with the condition of urinary tract infection.











 texto en
texto en