Introduction
Malignant hyperthermia (MH) is a critical event in anesthesiology. It is an autosomal dominant pharmaco-genetic syndrome of incomplete penetrance and variable aggressiveness, triggered by the exposure to depolarizing neuromuscular blockers and volatile anesthetics. It may have a fulminant onset and rapid course, with mortality rates close to 65% if a specific treatment is not administered.1 The prevalence of the MH episodes ranges from 1:10,000 up to 1:220,000 cases per anesthesia administered.2 In a study conducted in Bogotá, the estimated incidence was 1:65,000,3 while in Spain, the Carlos III Health Institute estimates and incidence of 1/14,000 cases in pediatric anesthesia and of 1/40,000 in adults.4 Notwithstanding its low incidence, the lethality of the condition makes it mandatory to develop competencies for managing the crisis, as timely identification and proper management reduce mortality to less than 10%.1 However, due its low frequency, the clinic dose not provide the proper setting for training, as there are not enough cases for a traditional training. Furthermore, such mortality rates represent a very narrow margin of error and the consequences are unacceptable. Hence, developing simulation scenarios is an attractive option to develop the necessary skills when facing a potential crisis of MH. The anesthesiologist could respond efficiently to a potential real-life event, if adequately trained in a controlled and safe environment.
These simulation scenarios allow for making mistakes and understanding the consequences, with the possibility of repeating the procedure based on the feedback received. The use of simulators is in fact an accepted methodology, and its use is encouraged in medicine.5 Although the studies that have evaluated the benefits of simulation to develop competencies are not yet rigorous enough, the current evidence shows the importance and the potential benefits of simulation scenarios as part of medical training.6,7
Chopra et al8 showed that anesthetists trained under a simulation model for MH respond faster, adhere more closely to the management guidelines, and their performance is better as compared against anesthesiologists who did not receive the training.
The availability of systems to simulate cases of MH is particularly interesting to develop skills in the management of a critical event during which the anesthetist is mostly liable for making the diagnosis and administering initial treatment.
Dantrolene, why should we simulate its reconstitution?
Dantrolene is the only available agent in the clinic for the specific treatment of MH; its administration is essential in managing a crisis, and the reconstitution and preparation of the agent is a high-priority procedure when facing a crisis. Ideally, both the anesthesiologists and the nursing staff should have the knowledge to handle the medication.
A close relationship has been established between the time elapsed from the first sign of the crisis and the administration of dantrolene, with higher probability of complications from MH as time passes; proper monitoring, with emphasis in capnography and temperature, together with the prompt administration of dantrolene, prevents complications, and lowers mortality.9,10 It has been shown that the risk of cardiac arrest is directly related to time, from the contact with the trigger and the start of therapy4; therefore, the dexterity and readiness to react in front of a crisis is a determining factor in a patient's survival.
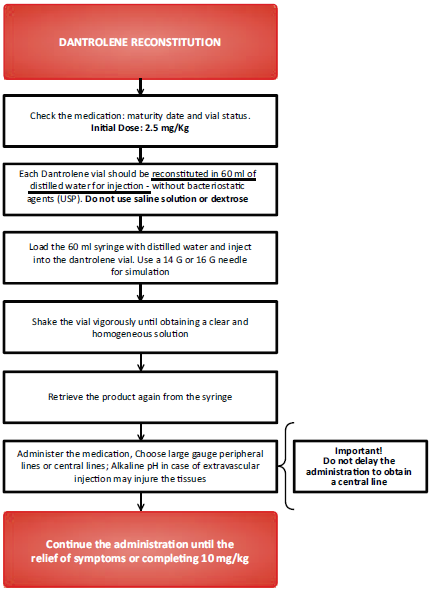
The most widely commercialized presentation of dantrolene are the 20 mg vials of lyophilized dantrolene, with 3 g of mannitol and sodium hydroxide, to ensure a pH of 9.5. This preparation must be reconstituted in 60 ml of distilled water. This is a highly lipophilic drug, with low solubility in water,10 which makes the reconstitution difficult. The simulation scenarios have already identified the difficulty to dissolve the drug in distilled water as a critical point; the process may take up to 4 minutes per vial.11 Keeping in mind the initial dose of 2.5 mg/kg, a 70-kg patient will need 9 vials just for the initial dose, requiring the effort of 3 of 4 full-time people. The lack of clarity about the process delays the start of therapy with a negative impact on the patient's outcome in the short and medium term.4,12
Therefore, the recommendation is to be knowledgeable and have experience in doing the reconstitution to reduce the preparation time and promptly administer the medication. The solution must be vigorously stirred until it becomes clear, with no visible particles before adminis-tration.10 The agility to reconstitute is essential. The initial dantrolene dose of 2.5 mg/kg must be repeated every 15 minutes until the symptoms improve, with a maximum accumulated dose of 10 mg/kg.1,13 So, in a worst case scenario, an average 70-kg patient would need 36 vials administered over the first hour of the crisis.
In addition, Dantrium (Intravenous, PAR pharmaceutical, Parkdale Road, MI, USA), the brand sold in Colombia and Spain, is distributed in 12 vial kits at a cost of $5,400,000 Colombian pesos (COP), which means a unit cost per vial of $450,000 COP. In Spain, the cost of treatment is 3000€.4 Therefore, wasting a vial due to wrongful reconstitution (eg, using dextrose or saline solution), in addition to causing delays in managing the crisis, represents an important economic loss during patient care, and using the actual drug for training purposes could imply wasting a very costly drug that occasionally has limited availability.
The relevance of the reconstitution process is reflected in the guidelines of our society. The checklists for malignant hypertension crisis management developed by the Colombian Society of Anesthesiology and Resuscitation (S.C.A.R.E.) since 2013 (available at: www.hiperter miamaligna.co) suggest appointing 1 single individual to dilute dantrolene (any staff member present during the response to the crisis). A similar recommendation is given by Kollmann-Camaiora et al4 in their clinical care protocol for managing MH. This proves the priority nature of this task, which is extremely relevant and complex so as to appoint 1 person (or even several) responsible for the its implementation.
So, we believe that dantrolene reconstitution is a relevant tool to develop competencies for managing a crisis of MH. Following is a description of the development of a simulation model for dantrolene reconstitution, using simple, low cost, and widely available materials. This model may be used as part of high-fidelity models in MH for training purposes when dealing with one of the critical points in crisis management.
To whom is the simulation model addressed.?'
Although the simulation model is addressed to anyone involved in the management of a crisis of MH, regardless of their level of training, we emphasize the significant role played by the anesthesiologist in the reconstitution process. During the crisis management, the anesthesiologist becomes the team leader, using his/her aptitude and knowledge from other areas different for medication reconstitution. However, the anesthetist has the responsibility of instructing the rest of the participants in the management of the crisis, the correct preparation of the medication, thus ensuring the initiation of therapy.
Manufacturing a dantolene vial for simulation purposes
In order to prepare a simulation vial for reconstitution using distilled water, we shall use a glass container that can be capped with a rubber plug as the ones used in operating room most vials (pharmacy-type glass bottle). One hundred milliliters medication bottles may be recycled (eg, Paracetamol). The vial content will be a mix of gelatin, which is difficult to dilute in room temperature water, simulating in this manner the difficulty faced when reconstituting the actual medication, so it is necessary to vigorously shake the vial in order to achieve the reconstitution. In order to make it look exactly like the commercial presentation, a label with the insert used in the dandrolene vials shall be used. The rubber plug must firmly cap the bottle to prevent any leaks during the simulation. The rest of the utensils normally used during the drug reconstitution will be used.
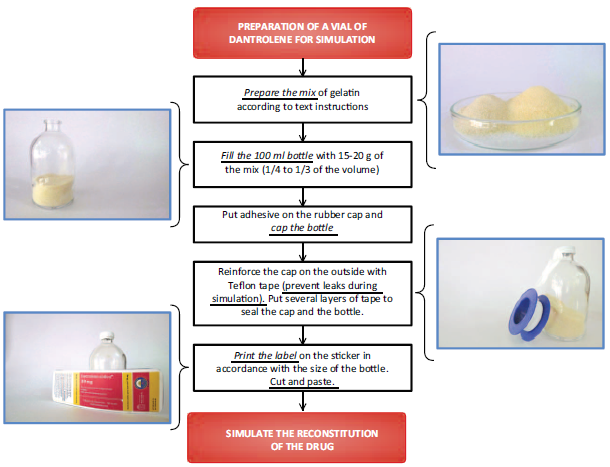
Materials to prepare a dantrolene reconstitution simulation kit (Fig. 1):
(1) Dantrolene vial for simulation:
Glass container (pharmacy-type bottle) of 60 or 100 ml: these containers are sold in perfume suppliers, the chemical industry, or manufacturers of glass products. These are low cost and easily available. The drug presentation is in 70 ml vials; however, 100 ml glass bottles are more easily available.
Rubber plug: these are collected from used medication vials. In our setting, the cephalexin or ampicillin-sulbactam vials are suitable for collecting the rubber caps. You just need to remove the metal strip securing the plug and the cap can then be easily removed.
Teflon tape: used by plumbers to prevent water leaks or to reinforce the metallic bands that secure actual vials. These are available in hardware stores.
Polychloroprene glue (eg, Boxer, Escobar y Martínez S.A, Bogotá DC, Colombia) or cyanoacrylate adhesive (eg, Super Bonder, Loctite, Westlake, OH, USA). The purpose of these adhesives is to further secure the rubber cap to the bottle, as the metallic band that usually secured the cap is not available. This is to avoid uncapping during injection of the distilled water or stirring of the bottle. We have achieved better results with cyanoacrylate-based adhesives. Another option is the use of hot-melt adhesives, silicon glue, or silone-based adhesive/sealant.
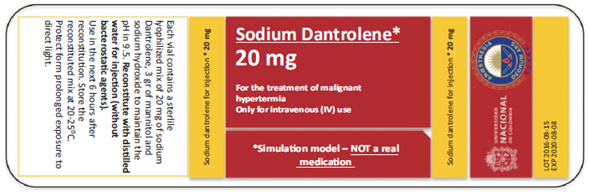
Label (Fig. 2): we provide the label model that can be printed in stickers to place on the bottles and simulate the original presentation of the drug. In the bottles used in the attached pictures, size used was 15 cm wide x 5 cm high.
Gelatin: 15 g of unflavored gelatin 70 g of yellow or orange gelatin (eg, pineapple flavor).
Emulsifier (optional): Glycerol Monostearate,30g. Available at chemical supplies stores.
Source: Authors.
Figure 2 Label for simulation vial. The size for printing shall fit the size of the glass container.
Supplemental material for the simulation:
(1). 60-ml syringe
(2). 14 G to 16 G needle: the mix is highly viscous and tends to solidify after 10 minutes; smaller gauge needles make the retrieval of the reconstituted model difficult.
(3). Bagged or bottled distilled water.
Preparation of a simulation vial
Prepare a mix of yellow gelatin and flavorless gelatin in a 1:4 to 1:5 ratio. Glycerol monostearate is optional (improves the solubility of the mix). If an electronic scale is available (can be bought for a low price), the amounts suggested above can be mixed.
Figure 3 is a step-by-step description of the preparation of the simulation model.
Once the vial has been prepared, we can simulate the reconstitution of a dantrolene vial (see Fig. 4) using the other components in the kit. Figure 5 illustrates how the simulation vial looks like, ready for use.
Model limitations
Although our model helps in becoming familiar with the reconstitution of dantrolene, it is not perfect yet, and there is still room for improvement in order to meet the standards of high fidelity simulation. On the basis of this model, new mixes may be developed to more precisely simulate the behavior of the actual drug.
The major disadvantage is the high viscosity of the resulting mix and the difficulty to remove the mix from the vial. We insist on the need to use large gauge needles for the simulation and removing the fluid from the vial as soon as possible. A positive aspect associated with this limitation is that this may help to ratify the difficulties to solubilize the original lyophilized product, insisting on the need to the vial stir vigorously to obtain a clear and homogeneous fluid.
The second negative point is the launching of a new presentation, Ryanodex, developed by Eagle Pharmaceutical in 2015, which is more concentrated and more soluble in water than the traditional presentation. Each Ryanodex vial of 250 mg of dantrolene, only requires 5 ml of water for reconstitution. Its improved solubility, in addition to its higher concentration, bypasses the difficulties that gave rise to our model. Nevertheless, the cost per vial is considerable ($2300 USD) and it is not available in Latin America, so there is need to continue using the lyophilized presentation for reconstitution.14,15 For the time being, all Ryanodex distributors are in the United States (see list at: http://www.ryanodex.com/ordering - consulted on December 11, 2017) and Eagle Pharmaceutical still owns the patent, which makes it doubtful that this presentation will be available in our country.
Conclusion
MH is a critical event in anesthesia, which although rare, is potentially lethal. Using a simulation tool is extremely valuable developing the skills to confront a crisis. Dantrolene reconstitution plays a key role, as the administration of this drug in the shortest possible time is a priority. For this reason, exclusively dedicated staff is assigned to perform this task during the management of the crisis. We submit a simulation model that can be prepared with easily available materials in order to practice the skills for reconstitution of the drug.
Ethical responsibilities
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.











 text in
text in