Introduction
Postoperative pain control in breast cancer surgery has become one of the most important goals for anesthetists. Multiple tools are available for achieving pain control, including intraoperative multimodal analgesia and re gional techniques (interpectoral block (PEC 1) and pectoral nerv block (PEC 2), cutaneous branches block of the intercostal nerves (BRILMA), intercostal blocks, or paravertebral blocks). Ultrasound-guided erector spinae plane (ESP) block is an innovative, easy, safe, and fast technique that can provide good analgesia with a reduced need for opioid use. We present the case of a patient taken to mastectomy in whom ESP block for postoperative analge sia was performed.
Clinical case
A 50-year-old female patient, housewife, was admitted in the oncologic gynecology outpatient clinic of Santander University Hospital. The patient had an 8-year history of a mass in the right breast, initially managed as a fibroadenoma, which has been growing rapidly and progressively over the past 7 months, involving the entire breast, and associated with intense, debilitating pain. She brings a biopsy report of November 2016 with a result of a phyllodes tumor and no other remarkable prior findings, and a normal cervical cytology report of March 2017. Laboratory tests on admission included whole blood count showing a hemoglobin of 11.2mg/dL, with no leukocytosis or neutrophilia. On physical examination, the patient is found in an acceptable general condition, a weight of 62 kg, with the right breast completely displaced due to a large multilobulated tumor mass of approximately 20 cm in diameter (Fig. 1), with areas of ulceration and not active bleeding. Because of its size, the mass limits ambulation and is a source of constant pain. The patient was admitted for urgent mastectomy with flaps.
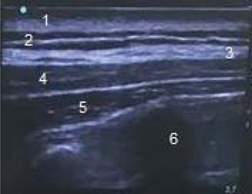
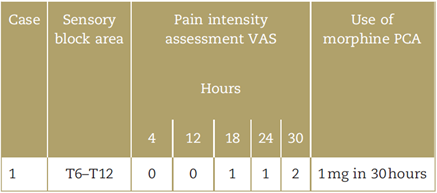
Two days later, the patient was transferred to the operating room for a right mastectomy plus axillary lymph node dissection. Basic monitoring was performed using a 3-channel electrocardiogram monitor, non-invasive blood pressure monitoring, and saturation; hypothermia was controlled using a thermal blanket. The Bispectral Index (BIS) was used for neurologic monitoring. Intravenous anesthesia induction was started with fentanyl 200 mg, propofol 120 mg, rocuronium 36 mg, and maintenance was achieved with balanced general anesthesia using sevo-flurane Minimum alveolar concentration (MAC) 0.6 to 0.7, remifentanil 0.15 to 0.2 mg/kg/minute, with dynamic settings for maintaining a BIS of 40 to 45. The gynecological oncology team performed right simple mastectomy plus axillary lymph node dissection and pectoralis major fascia resection and obtained a specimen of the right breast weighing 5020 g. During the procedure, the patient received dexamethasone 8-mg Intravenous (IV) for nausea and vomiting prevention, dipirone 2.5g and diclofenac 75-mg IV. At the end of the procedure, with the patient still under general anesthesia, the anesthesia team in charge of the case proceeded to the ESP block. The patient was placed on left lateral decubitus and, following asepsia and anti-sepsis, T6 to T7 and right paravertebral ultrasound was performed using a high-frequency linear probe, to identify the anatomy: (1) skin, (2) subcutaneous cellular tissue, (3) trapezius muscle, (4) rhomboid major muscle, (5) erector spinae muscle, and (6) transverse process (Fig. 2). A 50-mm echo-sensitive needle was placed through an in-plane cephalocaudal approach up to the erector spinae muscle, and bupivacaine with 0.25% epinephrine and 0.5% lidocaine was administered (total volume 20mL), achieving satisfactory erector spinae hydrodissection. The patient was also given intravenous morphine patient controlled analgesia for rescue analgesia. Assessment 4hours later found an area of anesthesia comprised by the right anterior hemithorax and axillary region and anesthesia from T4 to T12 in the posterior region. Pain assessment was performed over a 30-hour period using the analog visual scale (Table 1).
Discussion
This technique was originally described in 1905 by Sellheim and reintroduced into clinical practice by Eason and Wyatt in 1979. 1 There is an ongoing search for cost-effective strategies for postoperative pain control or for the control of acute or chronic pain syndromes.2
ESP block is an innovative technique in which local anesthetic is placed between the deep fascial plane of the erector spinae muscle and superficial to the tip of the transverse process. 3 Despite being a new technique, it has been shown to be useful in the treatment of acute or chronic conditions like chest, abdominal, and pelvic pain. 4
Results in our patient were found to be similar to those of other publications describing total anesthesia in the first 12hours, and even up to 36hours of chronic neuropathic chest pain4; moreover, this block offers immediate pain relief.
Among peripheral blocks, ESP is currently used as first-line postoperative analgesia in thoracotomy. 5 There are no studies in mastectomy, and it would be important to conduct further studies with a larger sample to replicate our results.
Based on our findings, ESP block may be recommended as an option or adjunct for pain management in this very important group of patients in our population.
Conclusion
ESP block is a safe, innovative strategy that is easy to perform and ensures good postoperative analgesia in radical mastectomy, reducing opioid requirements. It offers good pain management, contributing to faster patient recovery.
In this patient, the analgesic strategy using erector spinae block was efficient and provided 30hours of good analgesia with the need for only 1mg of morphine over 28hours, with no adverse effects or complications. These data suggest that ESP is a useful, simple, and fast strategy for postoperative pain management in mastectomy cases, although not many articles have been published to date on this topic.
Acknowledgments
We wish to thank Universidad Industrial de Santander and Hospital Universitario de Santander for making it possible for us to conduct our research.
Ethical responsibilities
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.











 texto em
texto em