Introduction
Residual neuromuscular block is observed at the end of anesthesia and is confirmed with monitoring,1-3 defined as a train-of-four (TOF) ratio (ratio between the fourth and first TOF response) <90% is undesirable and leads to a poorer prognosis.4,5 Although neuromuscular block is a continuous variable that depends on the competitive balance between acetylcholine and non-depolarizing neuromuscular blocking agents (such as rocuronium, which allows rapid access to the respiratory tract and the maintenance of adequate muscle relaxation for each procedure)1,6 in the motor end plate, neuromuscular block has been simplified into 4 stages: intense block, TOF = 0 and post-tetanic count (PTC) = 0; profound block, TOF = 0 and PTC > 1; moderate block, TOF count = 1 to 3; and recovery, TOF ratio >90%.7 However, when considering dosage of sugammadex, most authors consider moderate block to begin with the reappearance of the second TOF response (T2).8,9
Sugammadex has shown itself to be more effective than traditional neuromuscular block reversing agents (anticholinesterases) with respect to time to disappearance of the residual block(10,11; it allows reversal from any level of block, has a better profile in terms of side effects and eliminates the need to administer other drugs simultaneously.12 The dose of sugammadex recommended for moderate blocks is 2 mg/kg.13 The recommended dose for reversal is the same in all cases, despite the considerable variability in the effect of rocuronium, substantial differences in the depth of moderate block (which can vary between a TOF count of 1 and a TOF ratio of 89%), and the discrepancies derived from the effects of rocuronium and sugammadex in function of their molecular weights.13 This has led numerous authors to try to adjust the dose of sugammadex in moderate neuromuscular block. There are studies that show that the dose recommended by the industry may be excessive, indicating that when lower doses are used intraoperative monitoring is essential to avoid recurarization.9,14,15
Decreasing the dose of sugammadex in moderate blocks, with intraoperative monitoring to allow the titration of sugammadex, would represent an economic advantage that could lead to the more widespread use of the drug. It would also mean increased safety in those patients who need reoperation, since the low dose of sugammadex would make it possible to use a normal dose of rocuronium. Monitoring has been shown to be beneficial for reducing postoperative complications16 and is recommended even when the usual dose of sugammadex is used.17
The objective of our study was to determine whether half the initially recommended dose of sugammadex (i.e., 1 mg/kg) is sufficient to reverse any moderate block (with the dose adjusted through monitoring to obtain complete reversal) and whether this reduced dose involves any significant changes with regard to time to reversal and patient safety.
Methods
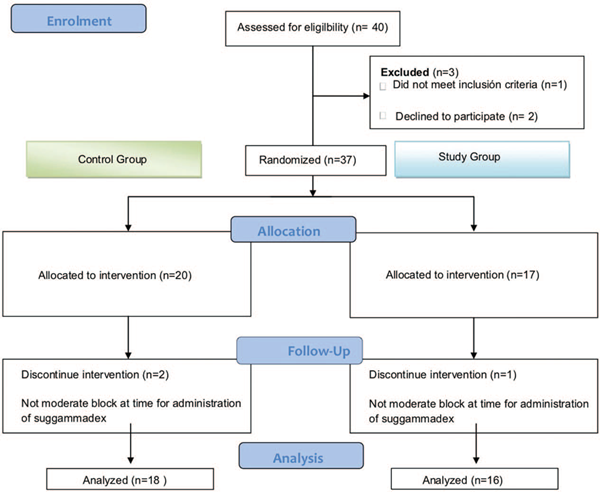
This was a phase IV unicenter clinical trial, no. EudraCT 2013-UU2362-39, approved by the ethics committee of our hospital (Informe del Comité Ético de Investigación Clínica del Parc de Salut Mar, Mayo 30 de 2013). The study was carried out between December 2013 and September 2015. The flow chart (Fig. 1) shows the distribution, randomization and loss-to-follow-up of patients who were enrolled in the study after having signed informed consent. Forty randomized patients were needed to obtain the 34 valid cases.
The randomization was performed using the block randomization model (MINSTD 1:1 at http://www.quantitativeskills.com/sisa/). The list generated with control cases and case studies was used in the pharmacy department, which prepared the blind syringes with the doses assigned by the randomization (20-mg/mL dose [control group] or a 10-mg/mL dose [study group] of sugammadex). The dose of sugammadex, random, and blind, was delivered to the operating room before the anesthetic induction for later use. We included patients scheduled for laparoscopic cholecystectomy under general anesthesia with traqueal intubation, performed by the same surgical team in all cases. Exclusion criteria were allergy or intolerance to some of the drugs used in the study, regular consumption of drugs that could interfere with the action of the neuromuscular blocking agents, end-stage kidney failure requiring replacement therapy, neurologic and/or neuromuscular disorders, age <18 years, and patient refusal. Standard induction of anesthesia was performed with the intravenous administration of midazolam (0.04 mg/kg), fentanyl (2 μg/kg), propofol (2mg/kg), and rocuronium (0.6 mg/kg).
Before the administration of the neuromuscular blocking agent, neuromuscular function was monitored using acceleromyography (TOF-Watch SX; Organon Ltd, Dublin, Ireland) with ulnar nerve stimulation using surface electrodes and the placement of the piezoelectric crystal on the first finger. A tetanic stimulation at 50 Hz was delivered and the supramaximal stimulus calculated once the signal was stabilized. Monitoring was performed with the following characteristics: duration of 0.2seconds at a frequency of 2 Hz and supramaximal intensity, repeated at 15-second intervals. The resulting contraction of the adductor pollicis muscle was recorded electronically using specific software (TOF-Watch SX Monitor v.1.1INT; Organon Ltd.) for subsequent calculations. The preparation and calibration sequence selection of the acceleromyograph were carried out according to the recommendations for correct neuromuscular monitoring, as defined in the guidelines of good clinical research practice in pharmacodynamic studies of neuromuscular blocking agents, drawn up as a result of an international consensus conference held in Copenhagen, revised and updated following a second consensus conference held in Stockholm in 2005.(3 In no case was normalization of the data necessary.
Anesthesia was maintained with a continuous infusion of propofol and bolus doses of fentanyl to obtain a depth of anesthesia at a bispectral index value of 45 to 60. We tried not to exceed an intraabdominal pressure of 12 mm Hg at any time. Bolus doses of rocuronium (0.15mg/kg) were used to maintain neuromuscular block with a TOF between 1 and 2. Before administration of the dose the state of blockade was recorded. After the operation, before extubation, the block was reversed using a blinded syringe, which could contain sugammadex, previously prepared and randomized by our hospital's pharmacy department. The dose to be administered was calculated as if all the syringes contained 20mg/mL, as per data sheet recommendations, that is, 2 mg/kg for a moderate block. If the block was intense or profound, the patient was excluded before administration of the dose. In this way, the anesthesiologist was blind to the dose administered. We collected demographic data, recovery time and intensity of neuromuscular block, rocuronium doses, and sugammadex doses.
Statistical analysis and sample size
According to the data sheet, after reappearance of T2 after rocuronium induced blockade (moderate blockade) the average time to recover the T4/T1 ratio to 0.9 after a 2 mg/kg dose of sugammadex is around 2 minutes. Sample size was calculated by a comparison of independent means. Accepting an alpha risk of 0.05 and a beta risk of 0.2, we obtained a sample of 16 subjects per group to detect a difference equal to or more than 2 minutes in recovery time from neuromuscular block. We assumed a common standard deviation of 2 minutes. We also estimated a loss-to-follow-up rate of 5%. For the statistical analysis, we used Student's test, Fisher's test and linear correlations. A P value <0.05 was considered significant.
Results
Table 1 shows the characteristics of the 34 patients. After randomization, 18 patients were assigned to the control group (usual dose of sugammadex) and 16 patients to the study group (half dose of sugammadex). No differences between the 2 groups with regard to patient characteristics were observed.
Table 1 Patient characteristics and intraoperative data.
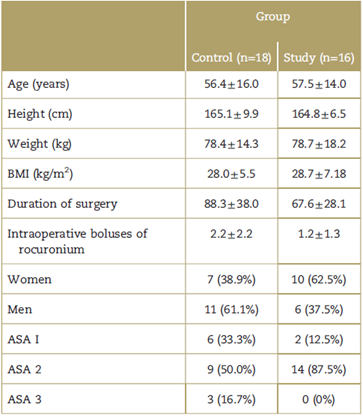
Data are expressed as mean ± standard deviation for continuous variables and as percentages for categorical variables. No significant differences were found between the groups. ASA, American Society of Anesthesiology score; BMI, body mass index.
Source: Authors.
During the intraoperative period, 73% of patients required a bolus dose of rocuronium to maintain the block below 2 TOF responses. Most patients (50.8%) received between 1 and 3 boluses of rocuronium: the median was 2, the 50% percentile, 2, and the mode 0. No supplementary boluses were required by 10.8% of patients in the control group and 16.2% of patients in the study group. The total dose of rocuronium was 64.2 ± 21.5 mg in the control group and 59.7 ± 19.8 mg in the study group.
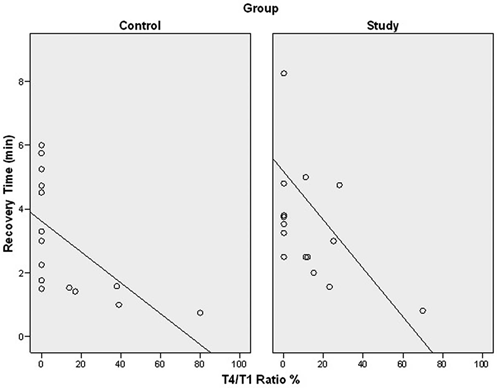
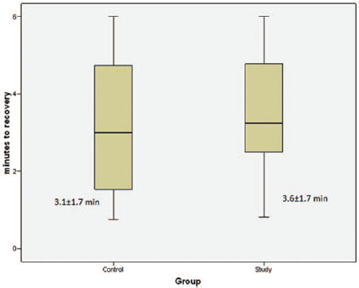
The intensity of the neuromuscular blocks of each group just before administration of sugammadex is shown in Table 2. The time to recovery of neuromuscular block after sugammadex is shown in Fig. 2, in which it can be seen that there were no differences between the 2 groups. Mean recovery time was 3.6±1.7 minutes for the study group and 3.1 ± 1.7 minutes for the control group. The mean difference was 0.49 minutes and its 95% confidence interval was not significant (P=0.42). Reversal of the block was complete with a single dose of sugammadex in all patients. Fig. 3 compares the relationship of depth of block to recovery time after administration of sugammadex between the 2 groups. There was a significant linear correlation between depth of block and recovery time in the 2 groups. We found no differences in time to recovery despite doubling the dose of sugammadex in the control group. The coefficient of variation of recovery time after sugammadex was 54.8% in the study group and 47.2% in the control group.
Table 2 Intensity of neuromuscular block just before administration of sugammadex.
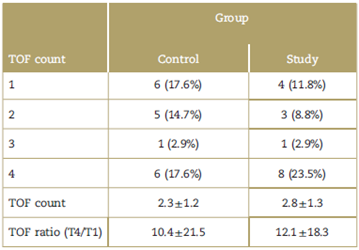
Neuromuscular block values before reversal with sugammadex. Data expressed as number ofcases and percentages for qualitative variables and mean ± standard deviation for quantitative variables. TOF count, number of responses to train-of-four; TOF ratio (T4/T1), as mean TOF ratio. No significant differences were found between the 2 groups. TOF=train-of-four.
Source: Authors.
Source: Authors.
Figure 2 Box plot showing time to recovery after administration of sugammadex and the mean time to recovery for study and control group. The diagrams represent the mean, standard deviation, and 95% confidence interval of the mean time to recovery in minutes. min = minutes.
Discussion
The present study shows that the dose of sugammadex can be reduced to half for the reversal of a moderate block with no loss of effectiveness or lengthening of the time to recovery with clinical repercussions, that is, reversal of a moderate block (most of the residual blocks at the end of an intervention are moderate)18 with sugammadex 1 mg/kg is just as effective as with sugammadex 2mg/kg. The difference in recovery time of 0.49minutes between the 2 doses is not clinically relevant.
Using high doses of sugammadex can have negative effects that should be considered. These potential risks are: allergies, increase in time of elimination, interactions, difficulty of managing neuromuscular blocking agents in cases of reoperation and an unnecessary increase in costs. It was initially recommended that rocuronium not be used until 24hours following the administration of sugammadex in patients with no renal dysfunction due to the elimination mechanism of the rocuronium-sugammadex complex.8,19 This time is increased in cases of renal insufficiency.20 Cammu et al21 later concluded that it was possible to obtain neuromuscular block again before 24 hours from the administration of sugammadex, although in their study the doses of rocuronium were higher and monitoring proved essential.
In terms of pharmacoeconomics, such monitoring would also make it possible to adjust the dose of sugammadex, reducing its economic impact. Moreover, sugammadex seems superior to other anticholinesterase drugs with respect to recovery time12; reversal from any depth of block22; safety profile regarding adverse effects23; the neostigmine might contribute to upper airway collapse24,25 and in the case of adjuvant drugs such as atropine may be produce tachycardia. Furthermore, some authors conclude that while some studies have shown that sugammadex has advantages in terms of recovery time and adverse effects,24,25 others have failed to find such differences.26 Nor is there agreement with respect to its economic advantage. While some authors find such an advantage, obtained chiefly by reducing recovery time in some circumstances,27 it has been somewhat difficult, for economic reasons for systematic use.
When analyzing these pharmacoeconomic studies comparing sugammadex with traditional drugs, it should be kept in mind that their methodological approaches are not always consistent and that the tests used for economic evaluation are not always the appropriate ones. While currently available data suggest that the routine use of sugammadex could improve recovery times, some caveats need to be highlighted: (1) sugammadex appears to be cost-effective if the reduction in recovery time is obtained in the operating room rather than in the Post-Anesthesia Care Unit; (2) the reduction in recovery time does not necessarily guarantee an increase in the availability of time to increase surgical activity; (3) the cost-effectiveness observed in trials might not be obtained in daily clinical practice and on a regular basis.28 Similar pharmacoeconomic studies comparing rocuronium-sugammadex with succinylcholine in cases of difficult airway have led to the conclusion that sugammadex is economically viable for routine use.28
Adjusting the dose of sugammadex might mean a greater risk of recurarization and, in addition, an increase in the variability of response. To avoid recurarization, intraoperative monitoring of the neuro-muscular block is essential and extremely useful. There was great variability between individuals in our study with regard to the effect of rocuronium by the variation in the number of boluses administered. For this reason, we recommend intraoperative monitoring for correct dosing, as do most authors7,15,16 to reduce postoperative complications derived from the presence of residual block.25 Kaufhold et al,15 recently studied adjustments in the dosage of sugammadex and in the course of their study found that neostigmine is not effective for the reversal of moderate block. As for sugammadex, they concluded that in 95% of patients, the administration of a very small dose (0.5 mg/kg) is sufficient to reverse moderate block in less than 5 minutes. They found no evidence of recurrence of the neuromuscular block, but consider monitoring the block to be essential to ensure patients' safety. These results are consistent with those found in the present study.
It is clear that depth of block is key in determining the optimal dose of sugammadex. It would appear that the current reversal strategy, based on the patient's weight, is not the most appropriate, as complete reversal can be obtained with lower doses. Neuromuscular block is a continuous, its qualitative stratification can make us you lose information. For example, a moderate block with a T4/T1 ratio of 70% is different from a moderate block with a TOF of 2 and it is not logical to administer the same dose (2 mg/kg) to reverse both. For this reason, in the present study we included patients with moderate block in accordance with the Stockholm revisión3 and those who were in the initial recovery stage. Despite the heterogeneity in the degree of blockade, the same dose of sugammadex is recommended in daily practice. However, we believe that this heterogeneity in the sample should be reflected in differences in dosing and that the use of neuromuscular block monitoring is preferable to allow the dose of sugammadex to be adjusted to its effect. The loss of information resulting from qualitative stratification causes us to treat superficial and near-profound blocks in the same way. Through monitoring, it would be possible to administer a smaller dose (e.g.,1 mg/kg) and, depending on its effect, either continue or discontinue administration if residual block persists. We could also adjust the doses of rocuronium and sugammadex and, in addition, ensure that there is no residual block in those cases in which rocuronium is used again after reversal with sugammadex, as proposed by some authors.21
The present study has some limitations, among which is the failure to evaluate profound or intense blocks. It can be extrapolated that such cases would also require monitoring, although this was not analyzed in the present study. Another limitation is that we analyzed blocks in a single type of surgery (laparoscopic) and do not know whether in a different kind of surgery some other type of monitoring, analysis, or reversal might be indicated.
Although the sample size was not large enough to warrant making direct changes in the dosing of sugammadex, we do suggest adjusting the dose in accordance with the variability shown through intraoperative monitoring to avoid unnecessary overdosing.











 text in
text in