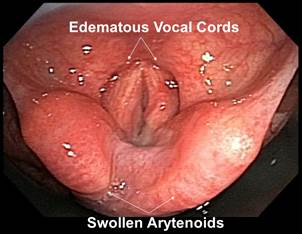
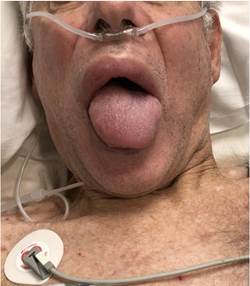
A 70-year-old male with metastatic cervical-spine-disease, orofacial edema andchronic pain presented for magnetic-resonance-imaging under general anesthesia. Prominent lip and tongue swelling (Image 1), and Mallampati-4 airway-grading prompted an awake-fiberoptic-intubation. Bronchoscopy revealed an edematous larynx (Image 2). After securing the airway, anesthesia was induced and no part of the glottis could be visualized on a check videolaryngoscopy. Prior anesthesia record documented a Mallampati-1 airway-grade and easy videolaryngoscopy-assisted intubation. Although initially his orofacial edema was erroneously attributed to metastatic disease, subsequent multidisciplinary consultation led to a diagnosis of Melkersson-Rosenthal syndrome. This rare syndrome is characterized by episodic attacks of facial swelling, facial palsy and fissuring of the tongue. However, this triad of major signs may not be present in all patients. Orofacial edema in these patients may take days to weeks to resolve. Antihistamines, corticosteroids, immunosuppressants and anti-inflammatory agents are often prescribed to treat the edema but definitive treatment remains unknown. Differential diagnoses include acquired or hereditary angioedema and drug or environmental allergies. Additionally, this syndrome can occur in conjunction with Crohn's disease and sarcoidosis. As it is necessary to rule out other causes of orofacial edema, diagnosis of Melkersson-Rosenthal syndrome is often delayed. 1,2 Patients typically start experiencing recurrent attacks of orofacial edema after their second decade of life. However, both the frequency and severity of attacks often decrease with increasing age. The prevalence of this syndrome is estimated at 0.08% and females are more likely to be afflicted than males.
Source: Authors.
Image 1 Prominent lip and tongue swelling, and Mallampati-4 airway-grading prompted an awake-fiberoptic-intubation.
Importantly, presence of orofacial edema with or without symptoms or signs such as dyspnea, dysphagia and stridor, should heighten suspicion for difficult airway management. Placement of and ventilation through a supraglottic airway device may be challenging in the presence of tongue and laryngeal swelling. Additionally, repeated laryngoscopy attempts may worsen edema and impair glottic visualization, potentially precipitating a "cannot intubate, cannot ventilate" circumstance. Consequently, prioritizing awake-fiberoptic-intubation with preparedness for obtaining speedy surgical airway access and/or instituting extracorporeal-membrane-oxygenation support may be prudent if patients present with acute facial swelling.3











 texto em
texto em