Introduction
Gallstone disease is more common in pregnant women as it is precipitated by the high hormonal influx (increased estrogen and progesterone), which favors a decrease in gallbladder motility and an increase in saturated cholesterol in the bile-physiopathological phenomena that facilitate calculi formation and its associated complications such as choledocholithiasis1. Gallstone disease during pregnancy is associated with preterm labor, neonatal and maternal morbidity, and an increase in maternal and neonatal readmission2. A prevalence of gallbladder stone disease during pregnancy is estimated between 3.3 % and 12 %3. Complications related to gallstones are common during pregnancy; in fact, it is the second indication for non-obstetric surgical intervention. An incidence of biliary sludge and cholelithiasis is estimated between 5 % to 31 % and 2 % to 11 %, respectively4. Complications of gallbladder stone disease during pregnancy, including cholecystitis, acute pancreatitis, and cholangitis, occur in about 10 %. The estimated incidence of choledocholithiasis is rare at 1/1000 pregnancies, and its resolution is achieved with endoscopic retrograde cholangiopancreatography (ERCP) in 100 % of cases of the reviewed series3-5.
These case reports were carried out following the CARE strategy (Case Report)6, which aims to illustrate how we currently have safe and effective bile duct intervention techniques in treating choledocholithiasis in pregnant women without exposure to fluoroscopy radiation.
Case 1
A 31-year-old patient with a history of mild preeclampsia, who is 27 weeks pregnant, is admitted for a 4-day clinical picture characterized by burning epigastric pain associated with oppressive pain in the dorsal and lumbar region. Concomitantly, she has multiple emetic episodes of food content and intolerance to the oral route. Upon physical examination, her blood pressure (BP) is at 113/69 mm Hg; heart rate (HR) 87 beats per minute (bpm); respiratory rate (RR) 18 breaths per minute (bpm); temperature (T) 36.2 °C; oxygen saturation (SaO2) 95 %; and weight 92 kg. Pink conjunctiva, icteric sclera, non-painful gravid uterus, without signs of peritoneal irritation, limbs without edema, without neurological deficit. Upon admission, paraclinical tests are taken, showing hyperbilirubinemia along with cholestasis (Table 1).
Table 1 Paraclinical tests upon admission for case 1
| Examination | Outcome | Units | Reference value |
|---|---|---|---|
| GOT-AST | 41 | U/L | 0-35 |
| GPT-ALT | 44 | U/L | 0-35 |
| Total bilirubin | 3.97 | mg/dL | 0.3-1 |
| Direct bilirubin | 2.73 | mg/dL | 0.0-0.2 |
| Indirect bilirubin | 1.24 | mg/dL | 0.0-1.1 |
| Creatinine | 0.46 | mg/dL | 0.5-1.0 |
| Amylase | 86 | U/L | 22-80 |
| Alkaline phosphatase | 215 | U/L | 30-120 |
ALT: Alanine aminotransferase; GPT: Glutamine pyruvic transaminase; AST: Aspartate aminotransferase; GOT: Glutamic oxaloacetic transaminase.
A cholangio-resonance is performed (Figure 1), documenting choledocholithiasis with obstructive effect and dilation of the intra- and extrahepatic bile duct and cholelithiasis with signs of cholecystitis. This indicates that the pregnant patient has cholelithiasis plus cholecystitis and choledocholithiasis. Therefore, it was decided to have her undergo an endoscopic ultrasound (EUS). ERCP. EUS is performed, which reveals the second portion of the duodenum with the usual appearance and the common bile duct of 6 mm diameter; in the middle portion, a hyperechoic image that projects a posterior acoustic shadow compatible with a calculus of 5 mm x 9 mm in diameter, and a distended gallbladder with multiple defects that generate a posterior acoustic shadow. In this sense, the result of the study is compatible with choledocholithiasis and cholelithiasis (Figure 2). Finally, the radial EUS is removed, and a duodenoscope is inserted.
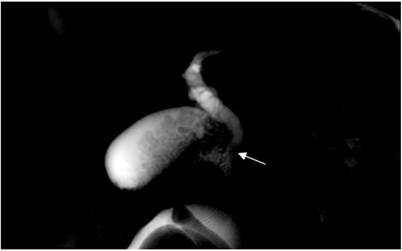
Figure 1 Cholangio-resonance. At the Vater’s ampulla level, a 6 x 4 mm defect (arrow) is observed in its lumen compatible with choledocholithiasis. Image property of the authors.
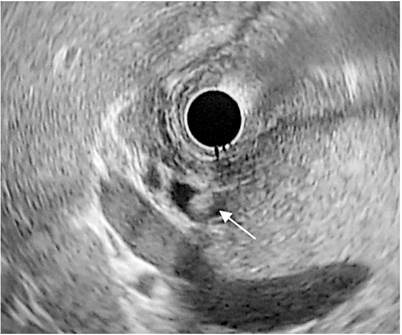
Figure 2 EUS prior to ERCP. Common bile duct of 6 mm, with a hyperechoic defect inside, which projects a posterior acoustic shadow of approximately 5 mm x 9 mm in diameter (arrow) compatible with choledocholithiasis. Image property of the authors.
Tokyo criteria apply for cholangitis:
Criterion A: it refers to the presence of systemic inflammation defined by fever > 38 °C, chills, or white blood cell count < 4000 or > 10 0007; this criterion was not met in this case.
Criterion B: it is defined as the presence of jaundice with bilirubin equal or greater than 2 or the alteration of liver function tests (transaminases, alkaline phosphatase, and gamma-glutamyl transferase elevated more than 1.5 times the normal upper limit; this criterion is met in this case7.
Criterion C: it describes the dilation of the bile duct by imaging or presence of an obstructive cause in the images (calculi, stenosis, stent)7; this criterion is met in this case.
After applying the Tokyo guidelines’ diagnostic criteria for cholangitis, it is concluded that this patient does not present a suspected or definitive diagnosis for cholangitis (Table 2).
Table 2 Diagnostic criteria for cholangitis
| Systemic inflammation |
| A-1 Fever (> 38 °C) or chills A-2 Inflammatory response in laboratories (leukocytes < 4000 µL or CRP > or = 1 mg/dL) |
| Cholestasis |
| B-1 Jaundice (total bilirubin > or = 2 mg/dL) B-2 Altered liver function tests (AP, GGT, AST, and ALT). Elevation more than 1.5 times the normal upper limit |
| Image |
| C-1 Dilation of the bile duct C-2 Evidence of etiology on imaging (stenosis, calculus, stent, etc.) |
| Diagnostic suspicion: an item A + an item B or C |
| Definitive diagnosis: one item in A + one item in B + one item in C |
AP: alkaline phosphatase; GGT: gamma-glutamyl transferase. Taken from: Tokyo Guidelines; 2018.
An ERCP is performed; the short-axis papilla is confronted with the arched papillotome and the hydrophilic guide, which shows the scant outflow of bile through the ampullary orifice. The papilla is then cannulated by directing the tip of the papillotome to the 11 o’clock meridian with an easy and deep advance of the guide about 5 cm. Subsequently, the hydrophilic guide is removed and then suctioned with the syringe until non-purulent bile fluid is obtained, confirming that the papillotome is in the bile duct (Figure 3). A wide papillotomy was performed without complications, and, later, a papillotome was exchanged by an extractor balloon. Then, the calculus is extracted. Finally, a new sweep is performed to extract bile without any other calculi. After the ERCP, a new EUS is performed to confirm that the common bile duct does not have lithiasis inside; thus, the pancreatic duct is not cannulated.
The patient is recovering satisfactorily, evidenced by the decreased bilirubin levels and the progressive decrease in transaminases (Table 3). On behalf of general surgery, laparoscopic cholecystectomy was scheduled to be performed in the same hospitalization-a procedure that had no complications. After this, the patient was discharged.
Case 2
A 37-year-old patient with a 31-week pregnancy, with no significant history, presents a clinical picture of approximately 2 months of evolution characterized by episodes of abdominal pain located in the right hypochondrium. 4 days before the consultation in our institution, the pain continued, which was associated with a fever of 38 °C and emesis of food content; these were the reasons for consultation. Upon admission, the physical examination shows BP 105/69 mm Hg; HR 66 bpm; FR 18 rpm; T 36.4 °C; and SaO2 94 %. Pink conjunctiva, sclera with jaundice tinge, moist oral mucosa, globose soft abdomen due to gravid uterus, pain on palpation in the right hypochondrium, without signs of peritoneal irritation, and eutrophic extremities without edema. The hepatic examination results show hyperbilirubinemia at the expense of direct bilirubin along with cholestasis (Table 4). A total abdominal ultrasound is performed, which shows dilation of the bile duct by 10 mm in diameter in its intra- and extrahepatic portion without identifying its cause, and biliary sludge and microlithiasis occupying the gallbladder neck without signs of acute cholecystitis. An intermediate probability choledocholithiasis was considered, and a cholangio-resonance was performed, which revealed dilation of the intra- and extrahepatic bile duct up to 11 mm. A 4 mm diameter defect is identified in the intraduodenal common bile duct lumen. The gallbladder has thin walls, and a 3-mm hypointense image is identified in its fundus. These findings are compatible with cholelithiasis and choledocholithiasis, without signs of acute cholecystitis (Figure 4).
Table 4 Paraclinical tests upon admission for case 2
| Examination | Outcome | Units | Reference value |
|---|---|---|---|
| GOT-AST | 36 | U/L | 0-35 |
| GPT-ALT | 31 | U/L | 0-35 |
| Total bilirubin | 2.29 | mg/dL | 0.3-1 |
| Direct bilirubin | 1.36 | mg/dL | 0.0-0.2 |
| Indirect bilirubin | 0.93 | mg/dL | 0.0-1.1 |
| Creatinine | 0.5 | mg/dL | 0.5-1.0 |
| Alkaline phosphatase | 121 | U/L | 30-120 |
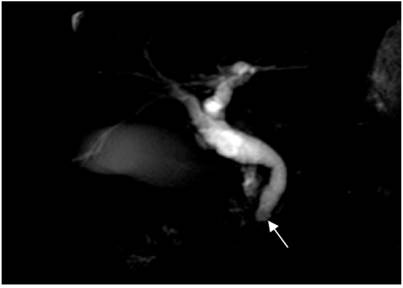
Figure 4 Cholangio-resonance. In the intraduodenal common bile duct, a 4 mm defect (arrow) is observed in its lumen compatible with choledocholithiasis. Image property of the authors.
It was decided to take the patient for a EUS-ERCP. An EUS is performed in which a normal-looking papilla is observed in the second duodenal portion. The common bile duct dilated up to 8 mm in diameter with multiple hyperechoic defects in its interior, approximately 2 mm to 5 mm, projecting a posterior acoustic shadow. The gallbladder shows cholelithiasis without cholecystitis, while the pancreas has a normal endosonographic appearance. The radial EUS is removed, then a duodenoscope is inserted (Figure 5).
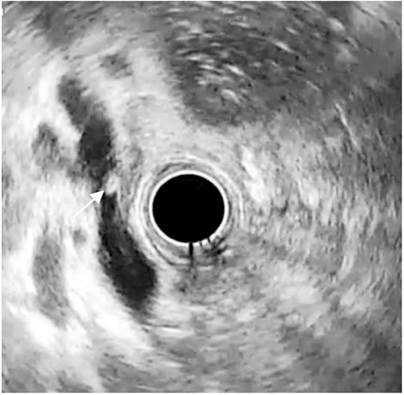
Figure 5 EUS prior to ERCP. Common bile duct dilated to 8 mm in diameter, with a hyperechoic defect in its interior of approximately 5 mm (arrow), which projects a posterior acoustic shadow compatible with choledocholithiasis. Image property of the authors.
An ERCP is performed using the same technique described with the previous patient (Figure 6). Fluoroscopy is not used to protect the fetus from radiation.
The procedure was carried out without complications. The patient evolved favorably in the postoperative period, with clinical and paraclinical improvement due to decreased bilirubin levels and the progressive decrease in transaminases (Table 5). She is scheduled to undergo an outpatient laparoscopic cholecystectomy.
Table 5 Paraclinical tests after ERCP for case 2
| Examination | Outcome | Units | Reference value |
|---|---|---|---|
| GOT-AST | 38 | U/L | 0-35 |
| GPT-ALT | 40 | U/L | 0-35 |
| Total bilirubin | 0.84 | mg/dL | 0.3-1 |
| Direct bilirubin | 0.32 | mg/dL | 0.0-0.2 |
| Indirect bilirubin | 0.52 | mg/dL | 0.0-1.1 |
| Alkaline phosphatase | 98 | U/L | 30-120 |
The Tokyo criteria for cholangitis were applied; in this patient, criteria B and C are met, so a diagnostic or definitive suspicion of cholangitis is not established (Table 2)7.
Discussion
Gallstone disease is a common condition in pregnant women, favored by decreased motility of the gallbladder. This results in less emptying associated with higher saturated cholesterol levels in the bile, contributing to increased lithogenesis. All these phenomena are triggered by progesterone and estrogens8.
Among the complications of biliary stone disease in pregnant patients is choledocholithiasis-a rare condition (incidence of 1/1000 pregnancies). Still, if not managed properly, it can lead to complications and morbidity, both maternal and fetal3,9.
In recent years, ERCP techniques without fluoroscopy have been implemented to prevent stochastic effects in the fetus. In 2009, Akcakaya et al described a series of cases of 6 pregnant patients who underwent ERCP without fluoroscopy. They reported that none of them presented post-ERCP complications, abortions, preterm births, or malformations in the fetus10.
In 2016, Ersoz et al published a series of retrospective cases of pregnant patients who underwent ERCP without radiation. It included 22 patients who underwent biliary sphincterectomy and pneumatic dilation with a balloon of the papilla. In this series, two patients had post-ERCP pancreatitis and gastrointestinal bleeding associated with the sphincterectomy. In all cases, pregnancy was normal and ended satisfactorily with the birth of a healthy child11. However, it is important to note that it achieves greater therapeutic success when EUS is associated with ERCP. This was demonstrated by Huang et al, who compared 32 pregnant women who underwent EUS-guided ERCP versus 36 pregnant women who underwent ERCP without EUS in 2013; findings were successful 90 % and 60 %, respectively12.
Recent studies provide new evidence on the safety of conventional ERCP with fluoroscopy in pregnancy, as demonstrated by Azad et al. In 2019, they conducted a systematic review and a meta-analysis that included 1307 pregnant patients who underwent ERCP with fluoroscopy and without fluoroscopy, in which no differences were found in terms of maternal or fetal complications13.
Stochastic effects on the fetus, attributed to radiation exposure, are possibly not evident in the different studies because they do not have sufficient follow-up time. However, the basic principle of radiological safety, As Low as Reasonably Achievable (ALARA), considers that there is no safe radiation level. Thus, radiation doses should always be given as low as possible to prevent stochastic effects in the future14.
It should be noted that the absence of radiation exposure in pregnant patients reduces the presentation of stochastic effects in the fetus14. For this reason, the combined EUS-ERCP technique is considered a choice to approach pregnant patients with choledocholithiasis since it does not expose the fetus to radiation-an event that potentially generates complications in the future. On the other hand, it allows locating calculi adequately in the common bile duct, verifying the resolution after ERCP, and greater therapeutic success than ERCP without EUS12,15. ERCP was not even considered in some series after a negative result for choledocholithiasis following a EUS15-17.
Currently, ERCP is an essentially therapeutic technique and is indicated for pregnant patients as a treatment for symptomatic choledocholithiasis, cholangitis, and biliary pancreatitis associated with persistent bile duct obstruction. Common risks associated with ERCP include duodenal perforation at 0.08 %-0.6 %, cholangitis at 0.5 % to 3 %, acute cholecystitis at 0.5 %, bleeding with a rate of 0.3 % to 2 %, and pancreatitis at 12 %. These complications can have consequences for the mother and fetus, and they occur with the same frequency in pregnant and non-pregnant women, as studies show.
Since postponing the procedure is associated with subsequent maternal and fetal complications, ERCP should not be postponed in patients with a clear indication3,18,19. Exposure to radiation during fluoroscopy while performing ERCP and its potential adverse effects on the product of pregnancy are among the greatest fears associated with the procedure for both physicians and patients. Stochastic results that occur regardless of the radiation dose received are the most worrying, as is the case of genetic alterations in the fetus and potential carcinogenesis (leukemias, childhood cancer, lymphomas, tumors of the central nervous system), which are present even with doses lesser than 100 mGy and are independent of the dose14. Effects that determine delays in fetus growth and cognitive development require higher doses than 100 mGv, which is a higher threshold dosage for the ERCP with fluoroscopy when performed by an expert, which is approximately from 0.1 to 3 mGv3.
Considering the stochastic effects of radiation associated with ERCP, the following measurements have been implemented to minimize radiation exposure of pregnant women during ERCP in recent years: using a lead apron to cover the maternal pelvis, using fluoroscopy as little as possible, and performing ERCP without fluoroscopy. Several studies have shown that implementing this technique is a safe and effective procedure in treating choledocholithiasis during pregnancy3,11,20.
When EUS is used along with ERCP, it effectively complements the calculi extraction procedure since it establishes their number and location before ERCP and after ERCP plus extraction. EUS evaluates the common bile duct and thus, confirms if its patency is adequate. On the other hand, some series have documented that after performing EUS, if no calculi are observed, ERCP is avoided16,17.
Conclusion
The study and treatment of pregnant women with choledocholithiasis require a detailed clinical approach, the appropriate indication and interpretation of laboratory and imaging studies, and the performance of bile duct intervention techniques that minimize fetal exposure to ionizing radiation allowing a reliable way to confirm the resolution of choledocholithiasis. These objectives are fully met by combining the EUS-ERCP technique. For this reason, our institution has the technology and trained personnel to carry out this type of intervention, which minimizes the risks for the mother and the fetus. Two cases of pregnant women with choledocholithiasis are described who underwent EUS-ERCP. During these interventions, there was no ionizing radiation exposure to the fetus, and the choledocholithiasis was successfully resolved without any complications for both mothers and children.











 texto en
texto en 





